Verapamil is a medication primarily used to treat high blood pressure, angina (chest pain), and certain heart rhythm disorders. It belongs to a class of drugs known as calcium channel blockers, which work by relaxing blood vessels and increasing the supply of blood and oxygen to the heart while reducing its workload. Verapamil is also sometimes prescribed off-label for other conditions, such as migraine headaches and cluster headaches.
Verapamil (Isoptin) is a rate-limiting calcium channel blocker that belongs to the non-dihydropyridine group like diltiazem.
Verapamil is listed in WHO's list of essential medicine.
It is used to treat the following conditions:
Angina:
- Immediate-release tablet:
- It is used to treat angina at rest, including unstable (crescendo, preinfarction) angina and vasospastic (Prinzmetal type) angina.
- It is also used in the treatment of chronic stable angina.
For rate control in Atrial fibrillation:
- Immediate-release tablet:
- In cases of persistent atrial flutter and fibrillation, it is used to regulate ventricular rate both at rest and during stress.
- Intravenous formulation:
- In atrial flutter and atrial fibrillation, it is utilised to temporarily regulate a fast ventricular rhythm.
- When atrial flutter and atrial fibrillation (Wolff-Parkinson-White and Lown-Ganong-Levine syndromes) are accompanied with accessory bypass tracts, it is not used.
Hypertension:
- Immediate-release tablet/ ER capsule and tablet:
- Additionally, it is employed to control hypertension.
- Guideline recommendations:
- In addition, 2017 Guidelines advise choosing thiazide-like diuretics or dihydropyridine calcium channel blockers over other medications if monotherapy is required in the absence of comorbidities (such as cerebrovascular disease, diabetes, chronic kidney disease, heart failure, ischemic heart disease, etc.) due to improved cardiovascular endpoints.
- Combination therapy is initially favoured in people at high risk and may be required to reach blood pressure objectives.
- When choosing a calcium channel blocker, the dihydropyridine class (such as amlodipine) is typically recommended over the non-dihydropyridine family, if tolerated (eg, diltiazem or verapamil).
Paroxysmal supraventricular tachycardia prophylaxis:
- Immediate-release tablet:
- Additionally, it is employed in the prevention of recurrent paroxysmal supraventricular tachycardia (PSVT).
- Supraventricular tachycardias:
- It is used to quickly restore paroxysmal supraventricular tachycardia to sinus rhythm, including those connected to accessory bypass tracts (Wolff-Parkinson-White and Lown-Ganong-Levine syndromes).
- Guideline recommendations:
- Acute conversion of a number of SVTs, including atrioventricular reentrant tachycardia (AVRT), atrioventricular nodal reentrant tachycardia (AVNRT), focal atrial tachycardia (AT), and multifocal atrial tachycardia (MAT) in patients with hemodynamic stability is also advised by ACC recommendations.
- For the continuous care of hemodynamically stable individuals with symptomatic supraventricular tachycardia (AVNRT, AVRT, focal AT, or MAT) without pre-excitation, who are typically not candidates for catheter ablation, oral verapamil is helpful and advised.
- For acute rate control in hemodynamically stable patients with atrial flutter, oral verapamil is also helpful.
Off Label Usage of Verapamil in Adults:
- It is used as off label agent in following
- Acute coronary syndrome (ACS)
- Cluster headaches
- Hypertrophic cardiomyopathy
- Idiopathic ventricular tachycardia
Verapamil (Isoptin) Dose in Adults
Verapamil Dosage in the treatment of Angina:
Immediate Release:
- Initial dose: 80 to 160 mg orally, taken 3 times daily.
- Note: The total daily dose may be adjusted based on individual response and tolerability.
Extended Release:
- When switching from immediate-release to extended-release formulations, the total daily dose usually remains the same unless formulation strength limits conversion.
Manufacturer's Labeling:
- The dosing information in the prescribing information may vary from current clinical practice.
- Typical dosing: 80 to 120 mg taken 3 times daily.
- For patients with increased sensitivity to verapamil (e.g., small stature): 40 mg taken 3 times daily.
- Maximum daily dose: 480 mg.
Verapamil Dosage in the treatment of Atrial fibrillation (rate control):
- Initial Bolus (Intravenous):
- 0.075 to 0.15 mg/kg administered over at least 2 minutes.
- Usual dose: 5 to 10 mg.
- If no response, an additional 10 mg bolus may be given after 15 to 30 minutes.
- If the patient responds to the initial or repeat bolus dose, a continuous infusion may be started.
- Continuous Infusion:
- Initial rate: 5 mg/hour.
- Titrate to achieve the target heart rate.
- Extended Release (Off-label Use):
- Usual maintenance dose: 180 to 480 mg orally once daily.
- Immediate Release:
- 240 to 480 mg orally daily, divided into 3 to 4 doses.
- Maximum daily dose: 480 mg.
Verapamil Dosage in the treatment of Cluster headaches:
Immediate Release:
- Initial dose: 240 mg, divided into 3 doses.
- Dose adjustment: Increase by 80 mg every 1 to 2 weeks until headaches subside or adverse reactions occur.
- Maximum dose: 960 mg per day.
- Some experts recommend electrocardiograms (ECGs) at baseline and after dose increases above 480 mg per day.
- Additional research may be needed to better understand the effectiveness of verapamil in treating cluster headaches.
Verapamil Dosage in the treatment of Hypertension:
Immediate Release:
- Usual dosage: 120 to 360 mg per day orally, divided into 3 doses.
- Maximum daily dose: 480 mg.
Extended Release (Calan SR, Isoptin SR):
- Initial: 180 mg orally once daily in the morning.
- For patients with increased sensitivity to verapamil (e.g., small stature): 120 mg once daily.
- If response is inadequate, dose may be increased weekly:
- Up to 240 mg once daily.
- Then 180 mg twice daily (or 240 mg in the morning followed by 120 mg in the evening).
- Maximum: 480 mg per day.
Extended Release (Verelan):
- Usual dosage: 240 mg orally once daily in the morning.
- For patients with increased sensitivity to verapamil (e.g., small stature): 120 mg once daily.
- If response is inadequate, dose may be increased weekly:
- Up to 480 mg once daily.
- Maximum: 480 mg per day.
Extended Release (Verelan PM):
- Usual dosage: 200 mg orally once daily at bedtime.
- For patients with increased sensitivity to verapamil (e.g., small stature): 100 mg once daily.
- If response is inadequate, dose may be increased weekly:
- Up to 400 mg once daily.
- Maximum dose: 400 mg daily.
Verapamil off Label Dosage in the treatment of Idiopathic ventricular tachycardia:
Intravenous (Off-label):
- 2.5 to 5 mg administered intravenously every 15 to 30 minutes.
Immediate Release:
- 360 mg per day orally, divided into 3 doses.
Extended Release:
- 240 to 480 mg orally once daily.
Verapamil Dosage in the treatment of PSVT prophylaxis:
Immediate Release:
- 240 to 480 mg orally daily, divided into 3 to 4 doses.
- Maximum daily dose: 480 mg.
Note: When transitioning from immediate-release to extended-release formulations, the total daily dose typically remains unchanged unless formulation strength limitations prevent equal conversion.
Verapamil Dosage in the treatment of Supraventricular tachycardia (ongoing management):
Immediate Release:
- Initial dose: 120 mg daily, divided into doses.
- Maximum maintenance dose: 480 mg per day, divided into doses.
Extended Release:
- Initial dose: 120 mg once daily.
- Maximum maintenance dose: 480 mg per day, taken once daily.
Verapamil Intravenous Off label dosage in the treatment of acute Supraventricular tachycardia (SVT):
ACLS Guidelines:
- Initial IV dose: 2.5 to 5 mg over 2 minutes (over 3 minutes in older patients).
- If no response, a second dose of 5 to 10 mg (~0.15 mg/kg) may be given 15 to 30 minutes after the initial dose.
- Maximum total dose: 20 to 30 mg.
ACC/AHA/HRS SVT Guidelines:
- IV dose: 5 to 10 mg (0.075 to 0.15 mg/kg) over 2 minutes.
- If no response, a second dose of 10 mg (0.15 mg/kg) may be given 30 minutes after the initial dose.
- Followed by an infusion at 0.005 mg/kg/minute.
Verapamil (Isoptin) Dose in Children
Verapamil Dose in the treatment of Supraventricular tachycardia (SVT):
Infants:
- IV: 0.1 to 0.2 mg/kg/dose (usual: 0.75 to 2 mg/dose); may repeat dose after at least 30 minutes if response inadequate.
- Note: Use with caution due to potential adverse effects. Continuous ECG monitoring and expert consultation are recommended.
Children and Adolescents (1 to 15 years):
- IV: 0.1 to 0.3 mg/kg/dose (usual: 2 to 5 mg/dose); maximum dose: 5 mg/dose; may repeat dose in 15 to 30 minutes if response inadequate; maximum dose for second dose: 10 mg/dose.
- Note: Consider intraosseous administration. Optimal interval for subsequent doses should be individualized.
Adolescents (≥16 years):
- Initial IV dose:
- PALS guidelines: 0.1 to 0.3 mg/kg/dose; maximum dose: 5 mg/dose.
- Manufacturer's labeling: 5 to 10 mg (0.075 to 0.15 mg/kg/dose); maximum dose: 10 mg/dose.
- Repeat dose: May repeat dose in 15 to 30 minutes if adequate response not achieved; maximum dose for second dose: 10 mg/dose.
- Note: Optimal interval for subsequent doses should be individualized.
Children and Adolescents (Limited Data):
- Oral immediate release: 2 to 8 mg/kg/day orally in 3 divided doses; maximum daily dose: 480 mg/day.
- Note: Dosage may vary based on individual response and should be closely monitored.
Verapamil Pregnancy Risk Factor: C
- Verapamil can affect the fetus if used during pregnancy, potentially causing issues like slow heart rate, heart block, or low blood pressure.
- However, for women with hypertrophic cardiomyopathy who are already using verapamil before pregnancy, it might be safe to continue, but close monitoring is essential.
- In pregnant women experiencing supraventricular tachycardia (SVT) with ineffective or contraindicated treatments like adenosine or beta-blockers, verapamil administered intravenously could be an option.
- It can also be used to manage SVT symptoms in highly symptomatic patients, with the smallest effective dose recommended, especially avoiding it during the first trimester if possible.
- Generally, it's preferable to avoid using verapamil for treating hypertension during pregnancy due to potential risks to both the mother and the baby.
- Other medications are usually preferred.
- For guidance on managing cardiovascular conditions during pregnancy, additional guidelines are available.
Verapamil use during breastfeeding:
- Verapamil and its metabolite norverapamil can be found in breast milk, but the amount transferred to the infant is very low, with the relative infant dose (RID) being less than 1% of the mother's dose per weight-adjusted dose.
- Generally, medications are considered safe for breastfeeding when the RID is below 10%.
- Studies following maternal use of verapamil at typical doses have not shown adverse effects in breastfed infants.
- Although some manufacturers advise against breastfeeding while using verapamil, it's generally considered compatible with breastfeeding according to the World Health Organization (WHO).
Verapamil dose in renal disease:
Manufacturer's Labeling:
- Oral (Verelan PM):
- Initial dose: 100 mg once daily at bedtime.
- Caution advised; additional ECG monitoring may be considered.
- Injection:
- No dosage adjustments provided.
- Repeated injections in patients with renal failure may lead to excessive effects; avoid if possible.
- If necessary, closely monitor blood pressure and PR interval, and use smaller repeat doses.
Alternate Recommendations:
- Studies suggest reduced clearance of verapamil in advanced renal failure.
- Some clinical papers report adverse effects in chronic renal failure patients at recommended doses.
- However, other studies show no difference in verapamil disposition between chronic renal failure and control patients in single-dose studies.
Dialysis:
- Verapamil is not removed by hemodialysis.
- Supplemental dose is not necessary.
Verapamil dose in Liver disease:
Oral:
- In Cirrhosis: Reduce dose to 20% of normal and monitor ECG.
- Calan, Calan SR, Verelan: Administer 30% of normal dose in severe hepatic impairment.
- Verelan PM: Initial dose: 100 mg once daily at bedtime.
Injection:
- No dosage adjustments provided.
- In Severe Impairment: Use with caution; consider additional ECG monitoring.
- In Cirrhosis: Reduce dose to 50% of normal and monitor ECG.
- Repeated injections in hepatic failure may lead to excessive effects; avoid if possible. If necessary, closely monitor blood pressure and PR interval, and use smaller repeat doses.
Common Side Effects of Verapamil Include:
- Central nervous system:
- Headache
- Gastrointestinal:
- Gingival hyperplasia
- Constipation
Less Common Side Effects of Verapamil Include:
- Cardiovascular:
- Peripheral Edema
- Hypotension
- Cardiac Failure
- Atrioventricular Block
- Bradycardia
- Flushing
- Angina Pectoris
- Atrioventricular Dissociation
- Cerebrovascular Accident
- Chest Pain
- Claudication
- ECG Abnormality
- Myocardial Infarction
- Palpitations
- Syncope
- Central Nervous System:
- Fatigue
- Dizziness
- Lethargy
- Pain
- Paresthesia
- Sleep Disorder
- Confusion
- Drowsiness
- Equilibrium Disturbance
- Extrapyramidal Reaction
- Insomnia
- Psychosis
- Shakiness
- Dermatologic:
- Skin Rash
- Alopecia
- Diaphoresis
- Erythema Multiforme
- Hyperkeratosis
- Macular Eruption
- Stevens-Johnson Syndrome
- Urticaria
- Endocrine & Metabolic:
- Galactorrhea
- Gynecomastia
- Hyperprolactinemia
- Spotty Menstruation
- Gastrointestinal:
- Dyspepsia
- Nausea
- Diarrhea
- Abdominal Distress
- Gastrointestinal Distress
- Xerostomia
- Genitourinary:
- Impotence
- Hematologic & Oncologic:
- Bruise
- Purpuric Vasculitis
- Hepatic:
- Increased Liver Enzymes
- Neuromuscular & Skeletal:
- Myalgia
- Arthralgia
- Muscle Cramps
- Weakness
- Ophthalmic:
- Blurred Vision
- Otic:
- Tinnitus
- Renal:
- Polyuria
- Respiratory:
- Flu-Like Symptoms
- Pulmonary Edema
- Dyspnea
Contraindication to Verapamil Include:
Oral:
- Do not use if:
- Allergic to verapamil or any part of the medication.
- Have severe left ventricular dysfunction or low blood pressure (systolic pressure <90 mm Hg) or cardiogenic shock.
- Have sick sinus syndrome (unless you have an artificial pacemaker).
- Have second- or third-degree atrioventricular (AV) block (unless you have an artificial pacemaker).
- Have atrial flutter or fibrillation and an extra electrical pathway in the heart (WPW syndrome, Lown-Ganong-Levine syndrome).
- Additional contraindications in Canadian labeling (not in US labeling):
- Complicated heart attack (with heart failure and lung congestion).
- Very slow heart rate, or using ivabradine.
IV:
- Avoid if:
- Allergic to verapamil or any part of the formulation.
- Have severe heart failure (unless caused by a certain type of fast heartbeat treatable with verapamil).
- Have severe low blood pressure or cardiogenic shock.
- Have sick sinus syndrome (unless you have an artificial pacemaker).
- Have second- or third-degree AV block (unless you have an artificial pacemaker).
- Taking IV beta-blocking agents.
- Have atrial flutter or fibrillation and an extra electrical pathway in the heart (WPW syndrome, Lown-Ganong-Levine syndrome).
- Have ventricular tachycardia.
- Additional contraindications in Canadian labeling (not in US labeling):
- Complicated heart attack (with heart failure and lung congestion).
- Severe left ventricular dysfunction.
- Very slow heart rate, using ivabradine, or breastfeeding.
Warnings and precautions
Conductivity abnormalities
- Verapamil can sometimes affect the electrical signals in the heart, leading to slower heartbeats like first-degree AV block or sinus bradycardia.
- In rare cases, more severe AV block or even asystole (a pause in the heart rhythm) may occur, especially in people with a condition called sick sinus syndrome.
- If there are signs of significant AV block, progression to more severe blockages, or certain types of bundle branch block, it's important to consider reducing the dosage or stopping the medication altogether.
Hepatic effects
- Verapamil can sometimes affect the liver, causing increased levels of liver enzymes like transaminases, alkaline phosphatase, and bilirubin.
- In some cases, it can lead to liver cell injury, which has been confirmed when the medication is stopped and then restarted.
- It's important to regularly check liver function while using verapamil.
- Although some elevations in liver enzymes may go away on their own while continuing the medication, it's essential to keep an eye on liver health.
Syncope and hypotension:
- Symptomatic low blood pressure with or without fainting may occur.
- Blood pressure should be lowered gradually based on the patient's condition.
- Accessory Bypass Tract (e.g., Wolff-Parkinson-White [WPW] syndrome):
- Verapamil can increase the conduction down the accessory pathway during atrial fibrillation or flutter, potentially leading to dangerous heart rhythms like ventricular fibrillation.
- It's important to avoid using verapamil in patients with this condition.
Arrhythmia:
- Verapamil is not recommended for patients with wide complex tachycardias unless the origin is known to be above the ventricles (supraventricular).
- Using verapamil in these cases can lead to severe low blood pressure upon administration.
Attenuated neuromuscular transmission
- Verapamil can sometimes reduce neuromuscular transmission, which may be concerning for patients with conditions like Duchenne muscular dystrophy or myasthenia gravis.
- Caution is advised when using verapamil in these patients, as dosage adjustment may be necessary to avoid complications.
Hepatic impairment
- Verapamil should be used cautiously in patients with liver problems, as dosage adjustment may be necessary.
- Monitor hemodynamics and possibly ECG in severe impairment.
- Avoid repeated injections of IV verapamil in patients with significant liver failure to prevent excessive effects.
Increased intracranial pressure
- IV verapamil has been associated with increased intracranial pressure in patients with tumors located above the tentorium (supratentorial tumors) during anesthesia induction.
- Exercise caution when using verapamil in these patients.
Left ventricular dysfunction:
- Verapamil should be used cautiously in patients with left ventricular dysfunction.
- Its negative effects on heart muscle contractions could worsen the condition.
- Avoid using verapamil in patients with heart failure, as it may not provide benefits and could lead to worse outcomes, according to ACCF/AHA guidelines.
Renal impairment
- Verapamil should be used cautiously in patients with kidney problems.
- Monitor hemodynamics and possibly ECG, especially in severe impairment, particularly if there's also liver impairment.
- Avoid repeated injections of IV verapamil in patients with significant renal failure to prevent excessive effects.
Verapamil: Drug Interaction
|
Abemaciclib |
Abemaciclib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Alcohol (Ethyl) |
Verapamil may raise the level of alcohol in the blood (Ethyl). |
|
Alfuzosin |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Aliskiren |
Aliskiren's serum levels may rise in response to verapamil. |
|
Alpha1-Blockers |
The hypotensive effects of calcium channel blockers may be strengthened. |
|
Amiodarone |
Amiodarone's bradycardic action may be enhanced by calcium channel blockers (Nondihydropyridine). Sinus arrest has reportedly occurred. |
|
AmLODIPine |
The serum levels of AmLODIPine may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Amphetamines |
May lessen the effectiveness of antihypertensive agents. |
|
Antipsychotic Agents (Second Generation [Atypical]) |
Antipsychotic drugs' hypotensive effects may be enhanced by blood pressure-lowering medications (Second Generation [Atypical]). |
|
Apixaban |
Apixaban's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
ARIPiprazole |
The serum levels of ARIPiprazole may rise in the presence of CYP3A4 Inhibitors (Moderate). Management: Keep an eye out for enhanced pharmacologic effects of aripiprazole. Depending on the concurrent therapy and/or the indication, aripiprazole dosage modifications may or may not be necessary. For detailed advice, refer to the complete interaction monograph. |
|
Aspirin |
Nondihydropyridine, a calcium channel blocker, may increase the antiplatelet action of aspirin. |
|
Atosiban |
Calcium channel blockers may intensify Atosiban's harmful or hazardous effects. Particularly, pulmonary edoema and/or dyspnea may be at higher risk. |
|
Barbiturates |
Calcium Channel Blockers' metabolic rate might be increased. Management: Keep an eye out for any diminished therapeutic effects of barbiturate medication when concurrently using calcium channel blockers. There may need to be dose modifications with calcium channel blockers. The concurrent use of phenobarbital and nimodipine is not recommended. |
|
Barbiturates |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Benperidol |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Benzhydrocodone |
The serum levels of Benzhydrocodone may rise in response to moderate CYP3A4 inhibitors. In particular, there might be an increase in hydrocodone concentration. |
|
Beta-Blockers |
Nondihydropyridine, a calcium channel blocker, may increase the hypotensive effects of beta-blockers. In addition, reports of bradycardia and heart failure symptoms have been made. The serum concentration of beta-blockers may rise in response to calcium channel blockers (nondihydropyridine). Levobunolol and metipranolol are exceptions. |
|
Blonanserin |
Blonanserin's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Bosentan |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Bosentan |
The serum levels of bosentan may rise after taking CYP3A4 Inhibitors (Moderate). Management: It is not advised to take a CYP2C9 and CYP3A inhibitor concurrently, or a single medication that inhibits both enzymes, with bosentan because this will likely result in a significant rise in the drug's serum level. Monograph for more information. |
|
Bradycardia-Causing Agents |
May intensify other bradycardia-causing agents' bradycardic effects. |
|
Brentuximab Vedotin |
The serum concentration of Brentuximab Vedotin may rise in response to P-glycoprotein/ABCB1 Inhibitors. More specifically, levels of the substance's active monomethyl auristatin E (MMAE) component might rise. |
|
Bretylium |
Bradycardia-Causing Agents' bradycardic effect might be enhanced. In patients taking AV blocking medications, bretylium may also strengthen atrioventricular (AV) blockade. |
|
Brexpiprazole |
Brexpiprazole's serum levels may rise in the presence of moderate CYP3A4 inhibitors. Treatment: If brexpiprazole is used with a moderate CYP3A4 inhibitor and a strong or moderate CYP2D6 inhibitor, or if a moderate CYP3A4 inhibitor is used in a CYP2D6 poor metabolizer, the dose should be lowered to 25% of the usual amount. |
|
Brimonidine (Topical) |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
BusPIRone |
The serum content of BusPIRone may rise in response to calcium channel blockers (Nondihydropyridine). |
|
Calcium Channel Blockers (Dihydropyridine) |
Possibly makes calcium channel blockers' hypotensive effects more potent (Nondihydropyridine). Calcium Channel Blockers (Nondihydropyridine) may cause an increase in serum calcium channel blocker concentration (Dihydropyridine). |
|
Calcium Salts |
May reduce calcium channel blockers' therapeutic efficacy. |
|
Cannabidiol |
Cannabidiol's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Cannabis |
Cannabis serum concentrations may rise in response to moderate CYP3A4 inhibitors. Serum concentrations of cannabidiol and tetrahydrocannabinol may rise particularly. |
|
Cardiac Glycosides |
The AVblocking effect of cardiac glycosides may be enhanced by calcium channel blockers (nondihydropyridine). Cardiac Glycosides' serum levels may rise in response to calcium channel blockers (Nondihydropyridine). |
|
Clofazimine |
May enhance the serum level of CYP3A4 substrates (High risk with Inducers). |
|
CloNIDine |
May improve Calcium Channel Blockers' ability to inhibit AV (Nondihydropyridine). Additionally, sinus node dysfunction might be aggravated. |
|
Clopidogrel |
Calcium channel blockers may reduce Clopidogrel's therapeutic efficacy. |
|
CloZAPine |
CYP1A2 Inhibitors (Weak) may raise the level of CloZAPine in the serum. Management: Separate drug interaction monographs go into further detail about the medications indicated as exceptions to this book. |
|
Codeine |
The active metabolite(s) of codeine may be present at higher serum quantities while taking CYP3A4 Inhibitors (Moderate). |
|
CYP3A4 Inducers (Moderate) |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
CYP3A4 Inhibitors (Moderate) |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
CYP3A4 Substrates (High risk with Inhibitors) |
The metabolism of CYP3A4 Substrates may be decreased by moderate CYP3A4 Inhibitors (High risk with Inhibitors). Alitretinoin (Systemic), Praziquantel, Trabectedin, and Vinorelbine are exceptions. |
|
Deferasirox |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Dexmethylphenidate |
May lessen the effectiveness of antihypertensive agents. |
|
Diazoxide |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Dronabinol |
Dronabinol's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
DULoxetine |
The hypotensive impact of DULoxetine may be enhanced by blood pressure lowering medications. |
|
Duvelisib |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Efavirenz |
Calcium Channel Blockers' serum concentration can drop. |
|
Erdafitinib |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Erdafitinib |
May enhance the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Erdafitinib |
P-glycoprotein/ABCB1 Substrates serum levels can rise. |
|
Estrogen Derivatives |
The serum concentration of oestrogen derivatives may rise in response to moderately potent CYP3A4 inhibitors. |
|
Fexofenadine |
Fexofenadine's serum levels may rise in response to verapamil. |
|
Fingolimod |
Verapamil may increase Fingolimod's bradycardic effects. |
|
Flecainide |
Verapamil may intensify Flecainide's harmful or hazardous effects. This combination may drastically reduce AV nodal conduction and myocardial contractility, in particular. |
|
Fluconazole |
Calcium Channel Blockers' serum levels can rise. |
|
Fosnetupitant |
May enhance the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Grapefruit Juice |
Verapamil serum levels can rise. |
|
Halofantrine |
Halofantrine's serum levels may rise in response to moderate CYP3A4 inhibitors. Management: If halofantrine is taken with mild CYP3A4 inhibitors, extreme caution and potentially increased ECG monitoring should be required. Drugs marked as exclusions from this document are covered in separate monographs on drug interactions. |
|
Herbs (Hypertensive Properties) |
May lessen the effectiveness of antihypertensive agents. |
|
Herbs (Hypotensive Properties) |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
HYDROcodone |
CYP3A4 Inhibitors (Moderate) may raise the level of Hydrocodone in the blood. |
|
Hypotension-Associated Agents |
The hypotensive action of hypotension-associated agents may be strengthened by blood pressure lowering medications. |
|
Ifosfamide |
The active metabolite(s) of ifosfamide may be present in lower serum concentrations when CYP3A4 Inhibitors (Moderate) are used. |
|
Imatinib |
Imatinib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Lacosamide |
Bradycardia-Causing Substances may intensify Lacosamide's AV-blocking effects. |
|
Larotrectinib |
May enhance the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Larotrectinib |
P-glycoprotein/ABCB1 Inhibitors may raise larotrectinib's serum levels. |
|
Levodopa-Containing Products |
Levodopa-Containing Products' hypotensive effects may be strengthened by blood pressure-lowering medications. |
|
Lithium |
Nondihydropyridine, a calcium channel blocker, may increase lithium's neurotoxic effects. Nondihydropyridine, a calcium channel blocker, may raise the serum levels of lithium. With this combination, lower or unchanged lithium concentrations have also been noted. |
|
Lormetazepam |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Magnesium Salts |
Calcium channel blockers might make magnesium salts more harmful or poisonous. Calcium Channel Blockers' hypotensive effects may be strengthened by magnesium salts. |
|
Manidipine |
Manidipine's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
MetFORMIN |
Verapamil may lessen MetFORMIN's therapeutic impact. |
|
Methylphenidate |
May lessen the effectiveness of antihypertensive agents. |
|
Midodrine |
Bradycardia-Causing Agents' bradycardic effect might be enhanced. |
|
Mirodenafil |
The serum concentration of Mirodenafil may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Molsidomine |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Naftopidil |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Naldemedine |
Naldemedine's serum levels may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Naldemedine |
The serum concentration of Naldemedine may rise in response to P-glycoprotein/ABCB1 Inhibitors. |
|
Nalfurafine |
Nalfurafine's serum levels may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Netupitant |
May enhance the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Neuromuscular-Blocking Agents (Nondepolarizing) |
The neuromuscular-blocking impact of neuromuscular-blocking agents may be enhanced by calcium channel blockers (Nondepolarizing). |
|
Nicergoline |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Nicorandil |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
NiMODipine |
NiMODipine's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Nintedanib |
Combination CYP3A4 and P-glycoprotein inhibitors may raise the level of Nintedanib in the blood. |
|
Nitroprusside |
Nitroprusside's hypotensive impact may be strengthened by blood pressure-lowering medications. |
|
Opioids (Anilidopiperidine) |
Calcium Channel Blockers' bradycardic impact might be boosted (Nondihydropyridine). Anilidopiperidine, a kind of opioid, may increase the hypotensive effects of calcium channel blockers (Nondihydropyridine). |
|
OxyCODONE |
Pglycoprotein/ABCB1 Substrates serum levels can rise. P-glycoprotein inhibitors may also make it easier for p-glycoprotein substrates to reach particular cells, tissues, and organs where p-glycoprotein is abundant (e.g., brain, T-lymphocytes, testes, etc.). |
|
Palbociclib |
May enhance the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Pentoxifylline |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
P-glycoprotein/ABCB1 Inhibitors |
Pglycoprotein/ABCB1 Substrates serum levels can rise. P-glycoprotein inhibitors may also make it easier for p-glycoprotein substrates to reach particular cells, tissues, and organs where p-glycoprotein is abundant (e.g., brain, T-lymphocytes, testes, etc.). |
|
P-glycoprotein/ABCB1 Substrates |
The serum concentration of P-glycoprotein/ABCB1 Substrates may rise in response to P-glycoprotein/ABCB1 Inhibitors. P-glycoprotein inhibitors may also make it easier for p-glycoprotein substrates to reach particular cells, tissues, and organs where p-glycoprotein is abundant (e.g., brain, T-lymphocytes, testes, etc.). Loperamide is an exception. |
|
Pholcodine |
Pholcodine's hypotensive impact may be strengthened by blood pressure lowering medications. |
|
Phosphodiesterase 5 Inhibitors |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Pimecrolimus |
The metabolism of pimecrolimus may be decreased by moderate CYP3A4 inhibitors. |
|
Propafenone |
Propafenone's serum levels may rise when taking CYP3A4 Inhibitors (Moderate). Management: Separate drug interaction monographs go into further detail about the medications indicated as exceptions to this book. |
|
Prostacyclin Analogues |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Prucalopride |
Prucalopride's serum levels may rise in response to P-glycoprotein/ABCB1 inhibitors. |
|
Quinagolide |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
QuiNIDine |
Verapamil's hypotensive effects should be improved. QuiNIDine's serum levels may rise in response to verapamil. |
|
Red Yeast Rice |
The blood content of Red Yeast Rice may rise in response to Calcium Channel Blockers (Nondihydropyridine). Particularly, levels of lovastatin (and perhaps other similar substances) may rise. |
|
Regorafenib |
Calcium Channel Blockers' bradycardic impact might be boosted (Nondihydropyridine). |
|
RifAXIMin |
The concentration of RifAXIMin in the serum may rise in response to P-glycoprotein/ABCB1 inhibitors. |
|
RisperiDONE |
RisperiDONE's serum levels may rise in response to verapamil. |
|
Rupatadine |
Rupatadine's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Ruxolitinib |
Bradycardia-Causing Agents' bradycardic effect might be enhanced. Treatment with roxolitinib Canadian product labels advise against using bradycardia-inducing substances as much as possible. |
|
Ruxolitinib |
Ruxolitinib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Salmeterol |
Salmeterol's serum levels may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Sarilumab |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
SAXagliptin |
The serum levels of SAXagliptin may rise in response to moderately potent CYP3A4 inhibitors. |
|
Sildenafil |
The serum concentration of Sildenafil may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Silodosin |
The serum concentration of Silodosin may rise in response to P-glycoprotein/ABCB1 Inhibitors. |
|
Silodosin |
Silodosin's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Siltuximab |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Tacrolimus (Systemic) |
Tacrolimus metabolism may be slowed down by calcium channel blockers (nonhydropyridine) (Systemic). |
|
Tacrolimus (Topical) |
Tacrolimus metabolism may be slowed down by calcium channel blockers (nonhydropyridine) (Topical). |
|
Tegaserod |
Tegaserod's serum levels may rise in response to P-glycoprotein/ABCB1 inhibitors. |
|
Terlipressin |
Bradycardia-Causing Agents' bradycardic effect might be enhanced. |
|
Tetrahydrocannabinol |
Tetrahydrocannabinol's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Ticagrelor |
Ticagrelor's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Tocilizumab |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Tofacitinib |
Bradycardia-Causing Agents' bradycardic effect might be enhanced. |
|
Trabectedin |
Trabectedin's serum levels may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Udenafil |
The serum levels of udenafil may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Vilazodone |
Vilazodone's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Vindesine |
Vindesine's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Yohimbine |
May lessen the effectiveness of antihypertensive agents. |
|
Zuclopenthixol |
The serum levels of Zuclopenthixol may rise in response to CYP3A4 Inhibitors (Moderate). |
|
Risk Factor D (Consider therapy modification) |
|
|
Acalabrutinib |
Acalabrutinib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Treatment: Lower the dose of acalabrutinib to 100 mg once daily while using a mild CYP3A4 inhibitor. If there is any concurrent use, keep a watchful eye on the patient for both acalabrutinib response and signs of side effects. |
|
Afatinib |
P-glycoprotein/ABCB1 Inhibitors may raise the level of Afatinib in the serum. Management: Reduce the dosage of afatinib by 10 mg, as directed per US labelling. If feasible, avoid combining drugs; if necessary, give the P-gp inhibitor together with or just after the afatinib dose. |
|
Amifostine |
Amifostine's hypotensive impact may be strengthened by blood pressure lowering medications. Treatment: Blood pressure-lowering drugs need to be avoided for 24 hours before amifostine is administered when used at chemotherapeutic doses. Amifostine should not be given if blood pressure lowering treatment cannot be stopped. |
|
Antifungal Agents (Azole Derivatives, Systemic) |
Calcium Channel Blockers' harmful or toxic effects could be exacerbated. In particular, itraconazole may make verapamil or diltiazem's unfavourable inotropic effects worse. Calcium Channel Blockers' metabolism may be slowed down by antifungal agents (systemic azole derivatives). Fluconazole and isavuconazonium, which are covered in different monographs, probably have less powerful effects than those of other azoles. Treatment: Itraconazole should not be used concurrently with felodipine or nisoldipine. With any such combination, regular monitoring is advised; calcium channel blocker dose decreases might be necessary. |
|
AtorvaSTATin |
Verapamil serum levels can rise. AtorvaSTATin's serum levels may rise in response to verapamil. When used with verapamil, management should take into account using lower atorvastatin dosages. |
|
Avanafil |
Avanafil's serum levels may rise in response to moderate CYP3A4 inhibitor therapy. Management: When used with a mild CYP3A4 inhibitor, the maximum adult dose of avanafil is 50 mg per 24 hours. Additionally, patients receiving this combination should be watched more attentively for signs of side effects. |
|
Betrixaban |
The serum concentration of betrixaban may rise in response to P-glycoprotein/ABCB1 inhibitors. Treatment: If betrixaban is used with a P-glycoprotein inhibitor, reduce the dose to an initial single dose of 80 mg, followed by 40 mg once day. |
|
Bilastine |
The serum concentration of bilastine may rise in response to P-glycoprotein/ABCB1 inhibitors. Management: When possible, look into alternatives; bilastine should be avoided in patients using p-glycoprotein inhibitors who have moderate to severe renal insufficiency. |
|
Brigatinib |
Brigatinib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: When possible, avoid taking brigatinib at the same time as mild CYP3A4 inhibitors. Reduce the brigatinib dosage by around 40% if such a combination cannot be avoided (ie, from 180 mg to 120 mg, from 120 mg to 90 mg, or from 90 mg to 60 mg). |
|
Bromocriptine |
The serum levels of bromocriptine may rise in response to moderately potent CYP3A4 inhibitors. Treatment: When used with a mild CYP3A4 inhibitor, the daily dose of bromocriptine should not exceed 1.6 mg. Other bromocriptine medicines do not give as detailed advice as the Cycloset brand does regarding dose restriction. |
|
Budesonide (Topical) |
The serum concentration of Budesonide may rise while using moderate amounts of CYP3A4 inhibitors (Topical). Management: Avoid this combination, according to US prescribing advice. Canadian goods labels do not expressly advise against anything. If used in conjunction, keep an eye out for too glucocorticoid effects as budesonide exposure may rise. |
|
CarBAMazepine |
The serum levels of CarBAMazepine may rise in response to calcium channel blockers (Nondihydropyridine). Calcium Channel Blockers' serum levels may be reduced by carbamazepine (Nondihydropyridine). Treatment: When starting nondihydropyridine calcium channel blockers, take into consideration reducing the dose of carbamazepine on an as-needed basis. Keep an eye out for carbamazepine's increased toxicity and the calcium channel blocker's diminished therapeutic benefits. |
|
Celiprolol |
Celiprolol's bradycardic action may be enhanced by verapamil. Celiprolol's serum levels may rise in response to verapamil. Treatment: It is not advised to use verapamil and celiprolol simultaneously, especially in patients who already have conduction issues. A drug-free interval is advised when transitioning from one agent to another, and heart rate should be constantly watched. |
|
Ceritinib |
Bradycardia-Causing Agents may intensify Ceritinib's bradycardic impact. Management: If this combination cannot be avoided, continuously monitor patients' blood pressure and heart rate throughout therapy and look for any signs of symptomatic bradycardia in them. A separate monograph is dedicated to discussing exceptions. |
|
Cilostazol |
Cilostazol's serum levels may rise in response to CYP3A4 Inhibitors (Moderate). Management: When treating adult patients who are already using mild CYP3A4 inhibitors, think about lowering the dose of cilostazol to 50 mg twice daily. |
|
Cimetidine |
Calcium Channel Blockers' serum levels can rise. Management: Take cimetidine substitutes into consideration. If there is no suitable substitute, watch for increased calcium channel blocker effects after starting or increasing the dosage of cimetidine and decreased effects after stopping or decreasing the dosage. |
|
Colchicine |
Colchicine's serum levels may rise after taking CYP3A4 Inhibitors (Moderate). Management: Increase monitoring for colchicine-related toxicity and decrease colchicine dose as advised when used with a moderate CYP3A4 inhibitor. For information, see the entire monograph. Patients with weakened liver or kidney function should be treated with extreme caution. |
|
Colchicine |
P-glycoprotein/ABCB1 Colchicine's serum levels may rise in response to inhibitors. It's possible that colchicine will distribute more widely throughout some tissues, like the brain. Treatment: Patients receiving a p-glycoprotein inhibitor and having compromised renal or hepatic function should not take colchicine. Colchicine dosage should be decreased in patients with normal renal and hepatic function as instructed. For information, see the entire monograph. |
|
CycloSPORINE (Systemic) |
Nondihydropyridine, a calcium channel blocker, may slow the metabolism of cycloSPORINE (Systemic). Calcium Channel Blockers may have slower metabolism when CycloSPORINE (Systemic) is taken (Nondihydropyridine). |
|
CYP3A4 Inducers (Strong |
May speed up CYP3A4 substrate metabolism (High risk with Inducers). Management: Take into account a substitute for one of the interfering medications. Specific contraindications may apply to some combinations. the relevant manufacturer's label. |
|
CYP3A4 Inhibitors (Strong) |
May slow down CYP3A4 substrate metabolism (High risk with Inhibitors) |
|
Dabigatran Etexilate |
The active metabolite(s) of dabigatran etexilate may be present in higher serum quantities when verapamil is used. Treatment: You might want to give dabigatran two hours before taking oral verapamil; you could also need to lower other doses. Regarding renal function, dabigatran indication, and US vs. Canadian labelling, different recommendations apply. Refer to the dabigatran labelling or the complete monograph. |
|
Dabrafenib |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). Management: When possible, look for substitutes for the CYP3A4 substrate. If concurrent therapy cannot be avoided, pay special attention to the substrate's clinical consequences (particularly therapeutic effects). |
|
Dapoxetine |
Dapoxetine's serum levels may rise in response to moderate CYP3A4 inhibitors. Treatment: When used with a mild CYP3A4 inhibitor, the daily dose of dapoxetine should be restricted to 30 mg. |
|
Deflazacort |
The active metabolite(s) of Deflazacort may be present in higher serum quantities when taking CYP3A4 Inhibitors (Moderate). When taking deflazacort with a strong or moderate CYP3A4 inhibitor, only take one-third of the prescribed dose. |
|
DOXOrubicin (Conventional) |
The serum concentration of DOXOrubicin may rise after using moderate amounts of CYP3A4 inhibitors (Conventional). Treatment: Whenever possible, avoid using mild CYP3A4 inhibitors in patients receiving doxorubicin. Pfizer Inc., a U.S. manufacturer, advises against using certain mixtures. |
|
DOXOrubicin (Conventional) |
Inhibitors of P-glycoprotein/ABCB1 may raise DOXOrubicin's serum concentration (Conventional). Treatment: Whenever possible, avoid using P-glycoprotein inhibitors in patients receiving doxorubicin. Pfizer Inc., a U.S. manufacturer, advises against using certain mixtures. |
|
Dronedarone |
The AV-blocking activity of dronedarone may be enhanced by calcium channel blockers (nondihydropyridine). Dronedarone may have more electrophysiologic effects overall. The serum concentration of dronedarone may rise in response to calcium channel blockers (nondihydropyridine). Calcium Channel Blockers' serum levels may rise in response to dronedarone (Nondihydropyridine). Management: Verapamil and diltiazem are examples of nondihydropyridine calcium channel blockers that should be used at lower starting dosages. Calcium channel blocker dosage should only be increased after receiving ECG-based confirmation that the combination is well-tolerated. |
|
Edoxaban |
The concentration of Edoxaban in the serum may rise in response to P-glycoprotein/ABCB1 inhibitors. Management: For more, see the whole monograph. Patients taking edoxaban for venous thromboembolism in conjunction with specific P-gp inhibitors are advised to take it in lower doses. It is not advised to modify the dosage when using edoxaban for atrial fibrillation. |
|
Eletriptan |
Eletriptan's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: Eletriptan shouldn't be taken within 72 hours of a moderate CYP3A4 inhibitor. |
|
Eliglustat |
Eliglustat's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: There are specific situations when use should be avoided. For information, consult the entire medication interaction monograph. |
|
Encorafenib |
Encorafenib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: Whenever possible, refrain from taking moderate CYP3A4 inhibitors and encorafenib concurrently. Reduce the encorafenib dose before beginning to use the CYP3A4 inhibitor if concurrent administration is required. For information, see the entire monograph. |
|
Enzalutamide |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). Treatment: Enzalutamide should not be used concurrently with CYP3A4 substrates that have a limited therapeutic index. Enzalutamide use, like with the use of any other CYP3A4 substrate, should be done cautiously and under close observation. |
|
Eplerenone |
Eplerenone's serum levels may rise in response to CYP3A4 Inhibitors (Moderate). Management: Depending on the indication and foreign labelling, different doses of eplerenone should be used concurrently with mild CYP3A4 inhibitors. For information, consult the entire medication interaction monograph. |
|
Esmolol |
Esmolol's bradycardic action may be enhanced by calcium channel blockers (nondihydropyridine). Management: Giving one medication while the effects of the other are still present is not advised when giving IV verapamil or diltiazem with esmolol. Esmolol is labelled as contraindicated for usage if taken within 24 hours in Canada. |
|
Everolimus |
CYP3A4 Inhibitors (Moderate) may raise the level of Everolimus in the blood. For the majority of cases, everolimus dose decreases are necessary. For detailed dose modification and monitoring suggestions, consult the full monograph or prescription information. |
|
Everolimus |
CYP3A4 (Moderate) and P-glycoprotein inhibitors may raise the level of Everolimus in the blood. For the majority of cases, everolimus dose decreases are necessary. For detailed dose modification and monitoring suggestions, consult the full monograph or prescription information. |
|
FentaNYL |
The serum levels of FentaNYL may rise in response to CYP3A4 Inhibitors (Moderate). Management: After starting this combination, keep a watchful eye on the patients for a few days and alter the fentanyl dosage as necessary. |
|
Fosphenytoin |
Calcium channel blockers may raise the level of fosphenytoin in the blood. Monitoring for phenytoin toxicity while using a calcium channel blocker (CCB) at the same time or reduced phenytoin effects while stopping the CCB are the two management options. Check for diminished therapeutic effects of CCB. The Canadian labelling for nimodipine specifically forbids the use of phenytoin. |
|
GuanFACINE |
CYP3A4 Inhibitors (Moderate) may raise the level of GuanFACINE in the serum. When starting this combo, cut the guanfacine dose in half. |
|
Ibrutinib |
Ibrutinib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Treatment: While paired with mild CYP3A4 inhibitors, reduce ibrutinib dosage to 280 mg per day when treating B-cell malignancies. When treating graft versus host disease, keep a close eye on the patients and adjust the ibrutinib dosage as necessary based on side effects. |
|
Ivacaftor |
Ivacaftor's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: Ivacaftor dosage reductions are necessary; for complete monograph material and specific recommendations based on age and weight. When taking ivacaftor/lumacaftor with a mild CYP3A4 inhibitor, there is no need to change the dosage. |
|
Ivosidenib |
Ivosidenib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: Whenever feasible, refrain from combining ivosidenib with mild CYP3A4 inhibitors. Watch out for increased ivosidenib toxicity if taken in combination. Drugs that are specifically mentioned as exceptions are covered in further detail in their own drug interaction monographs. |
|
Lorlatinib |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). Management: Avoid taking lorlatinib at the same time as any CYP3A4 substrates for which even a small drop in serum levels of the substrate could result in therapeutic failure and negative clinical outcomes. |
|
Lovastatin |
Lovastatin's serum levels may rise in response to verapamil. Treatment: In patients on verapamil, start lovastatin at a maximum adult dose of 10 mg/day and do not go over 20 mg/day. Keep an eye out for any symptoms of HMG-CoA reductase inhibitor toxicity, such as myositis |
|
Lurasidone |
Lurasidone's serum levels may rise in response to moderate CYP3A4 inhibitors. Treatment: According to the US labelling for lurasidone, the dose should be cut in half and used with a mild CYP3A4 inhibitor. Some non-US labelling advises starting with 20 mg/day of lurasidone and limiting the dosage to 40 mg/day; concurrent use of grapefruit products should be avoided. |
|
Macrolide Antibiotics |
Calcium Channel Blockers' metabolic rate might be decreased. Use a noninteracting macrolide as a possible management strategy. The Canadian labelling for felodipine expressly advises against using it in conjunction with clarithromycin. Azithromycin (Systemic), Fidaxomicin, Roxithromycin, and Spiramycin are exceptions. |
|
MiFEPRIStone |
May elevate CYP3A4 substrates' serum concentration (High risk with Inhibitors). Management: During and two weeks after mifepristone treatment, reduce doses of CYP3A4 substrates and keep an eye out for elevated amounts or toxicity. Fentanyl, pimozide, quinidine, sirolimus, and tacrolimus should all be avoided. Cyclosporine should also be avoided. |
|
Mitotane |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). Treatment: When administered in individuals receiving mitotane, doses of CYP3A4 substrates may need to be significantly modified. |
|
Obinutuzumab |
The hypotensive effects of blood pressure-lowering medications may be strengthened. Management: Take into account temporarily stopping blood pressure-lowering drugs 12 hours before the start of the obinutuzumab infusion and keeping them off until 1 hour after the infusion is finished. |
|
Olaparib |
Olaparib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: If at all feasible, refrain from administering mild CYP3A4 inhibitors to patients receiving olaparib. Olaparib dosage should be decreased to 150 mg twice daily if such concomitant use cannot be avoided. |
|
Phenytoin |
The serum levels of phenytoin may rise when calcium channel blockers are used. Calcium Channel Blockers' serum levels may be reduced by phenytoin. Avoid combining nimodipine or nifedipine with phenytoin for management. With any concurrent use, keep an eye out for phenytoin toxicity and/or diminished calcium channel blocker effects. |
|
Pitolisant |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). Management: Pitolisant should not be used in conjunction with a CYP3A4 substrate that has a limited therapeutic index. When administered with pitolisant, other CYP3A4 substrates need to be checked more carefully. |
|
Protease Inhibitors |
Calcium Channel Blockers' metabolism might be slowed down (Nondihydropyridine). The risk of AV nodal blockage may rise with higher calcium channel blocker serum concentrations. Management: When feasible, avoid concurrent use. Check for CCB toxicity if used. Atazanavir's producer advises that a dose reduction of 50% for diltiazem be taken into consideration. Use of bepridil and saquinavir, tipranavir, and darunavir/cobicistat is not advised. |
|
Ranolazine |
The serum concentration of Ranolazine may rise in response to Calcium Channel Blockers (Nondihydropyridine). When used with diltiazem or verapamil, the dose of ranolazine should be restricted to no more than 500 mg twice daily. |
|
Ranolazine |
Ranolazine's serum levels may rise after taking CYP3A4 Inhibitors (Moderate). Treatment: In patients receiving mild CYP3A4 inhibitors concurrently, the adult ranolazine dose should be restricted to no more than 500 mg twice daily (e.g., diltiazem, verapamil, erythromycin, etc.). |
|
Rifamycin Derivatives |
Calcium Channel Blockers' serum concentration can drop. This predominantly affects calcium channel blockers used orally. Management: Using rifampin with certain calcium channel blockers is not advised according to the labelling in the US and Canada. Look up the relevant labelling. |
|
Rivaroxaban |
Rivaroxaban's serum levels may rise in response to P-glycoprotein and CYP3A4 (Moderate) inhibitors. Management: In patients with normal renal function, nothing needs to be done. In individuals with estimated creatinine clearances of 15 to 80 mL/min, US labelling advises against using it unless the potential benefits exceed the hazards. Different labels from other countries may exist. |
|
Simvastatin |
Simvastatin's serum levels may rise in response to verapamil. Management: When at all feasible, refrain from taking simvastatin and verapamil together. Simcor (simvastatin/niacin) should not be used since the fixed simvastatin doses in the product surpass the adult maximum dose of 10 mg/day when used jointly. |
|
Sincalide |
The therapeutic benefit of Sincalide may be reduced by medications that affect gallbladder function. Prior to using sincalide to induce gallbladder contraction, you should think about stopping any medications that can impair gallbladder motility. |
|
Siponimod |
Siponimod's bradycardic action may be enhanced by bradycardia-causing substances. Management: Steer clear of combining siponimod with medications that can slow your heart rate. |
|
Sirolimus |
The serum concentration of Sirolimus may rise after taking CYP3A4 Inhibitors (Moderate). Management: If sirolimus is taken with a mild CYP3A4 inhibitor, keep an eye out for elevated serum concentrations. Lower starting dosages of sirolimus or dose reductions of sirolimus will probably be needed. |
|
Sonidegib |
Sonidegib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: Whenever possible, refrain from taking moderate CYP3A4 inhibitors and sonidegib concurrently. Limit the use of CYP3A4 inhibitors to less than 14 days when concurrent usage cannot be avoided, and keep an eye out for sonidegib toxicity (particularly musculoskeletal adverse reactions). |
|
St John's Wort |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). Management: Take into account a substitute for one of the interfering medications. Specific contraindications may apply to some combinations. the relevant manufacturer's label. |
|
Stiripentol |
May elevate CYP3A4 substrates' serum concentration (High risk with Inhibitors). Management: Due to the increased potential for side effects and toxicity, stiripentol should not be used with CYP3A4 substrates that are thought to have a narrow therapeutic index. Use of stiripentol with any CYP3A4 substrate necessitates closer observation. |
|
Suvorexant |
Suvorexant's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Treatment: Suvorexant is administered at a dose of 5 mg per day to patients who are on a mild CYP3A4 inhibitor. If more dosage is required for effectiveness, the maximum amount per day is 10 mg. |
|
Talazoparib |
Talazoparib's serum levels may rise in response to verapamil. Management: Lower the dose of talazoparib to 0.75 mg once daily if concomitant use cannot be avoided. Increase the talazoparib dosage to the level used before the start of verapamil after a period of 3 to 5 times the half-life of verapamil. |
|
Telithromycin |
Verapamil's bradycardic effects could be boosted. Telithromycin might make Verapamil's hypotensive impact even stronger. |
|
Tezacaftor |
Tezacaftor's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Treatment: Tezacaftor/ivacaftor should be administered in the morning, every other day, when taken with mild CYP3A4 inhibitors. Every other day, on days when tezacaftor and ivacaftor are given alternately, ivacaftor alone should be administered in the morning. |
|
TiZANidine |
The concentration of TiZANidine in the serum may rise in response to CYP1A2 Inhibitors (Weak). Management: Whenever you can, stay away from these pairings. Tizanidine should be started at an adult dose of 2 mg and increased in 2 to 4 mg increments depending on the patient's reaction if combination use is required. Watch out for tizanidine side effects, such as increased effects. |
|
Tolvaptan |
Tolvaptan's serum levels may rise in response to CYP3A4 Inhibitors (Moderate). Management: When used with a mild CYP3A4 inhibitor, jynarque dosage must be adjusted. For more detailed advice, consult the complete interaction monograph or labelling. Samsca use should generally be avoided when moderate CYP3A4 inhibitors are present. |
|
Venetoclax |
Venetoclax's serum levels may rise in response to moderate CYP3A4 inhibitors. Management: In patients who need these combinations, lower the dose of venetoclax by at least 50%. |
|
Venetoclax |
Venetoclax serum levels may rise in response to P-glycoprotein/ABCB1 inhibitors. In patients who need concurrent treatment with P-glycoprotein (P-gp) inhibitors, consider reducing the dose of venetoclax by at least 50%. |
|
Zopiclone |
Zopiclone's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: If taken with a mild CYP3A4 inhibitor, the first adult dose of zopiclone shouldn't be more than 3.75 mg. If these medications are taken together, patients should be kept an eye out for any zopiclone toxicity symptoms. |
|
Risk Factor X (Avoid combination) |
|
|
Aprepitant |
Aprepitant's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Asunaprevir |
Asunaprevir's serum levels may rise in response to moderate CYP3A4 inhibitor therapy. |
|
Bosutinib |
Bosutinib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Bromperidol |
The hypotensive impact of bromperidol may be enhanced by blood pressure lowering medications. Blood Pressure Lowering Agents' hypotensive effects may be lessened by bromperidol. |
|
Budesonide (Systemic) |
The serum concentration of Budesonide may rise while using moderate amounts of CYP3A4 inhibitors (Systemic). |
|
Cobimetinib |
Cobimetinib's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Management: Steer clear of combining cobimetinib with mild CYP3A4 inhibitors. Reduce the dosage of cobimetinib to 20 mg per day if concomitant short-term (14 days or less) use cannot be avoided. |
|
Conivaptan |
May elevate CYP3A4 substrates' serum concentration (High risk with Inhibitors). |
|
Dantrolene |
May make calcium channel blockers' hyperkalemic impact stronger (Nondihydropyridine). Dantrolene may intensify Calcium Channel Blockers' adverse inotropic impact (Nondihydropyridine). Management: Only intravenous dantrolene administration has been used to characterise this interaction. |
|
Disopyramide |
Verapamil may intensify Disopyramide's harmful or hazardous effects. The possibility for severe myocardial contractility depression is particularly concerning. Management: It is best to avoid taking disopyramide at the same time 48 hours before or 24 hours after taking verapamil. |
|
Dofetilide |
Dofetilide's serum levels may rise in response to verapamil. |
|
Domperidone |
Domperidone's serum levels may rise in response to moderate CYP3A4 inhibitors. Management: Separate drug interaction monographs go into further detail about the medications indicated as exceptions to this book. |
|
Flibanserin |
Flibanserin's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Fosaprepitant |
Fosaprepitant's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Fusidic Acid (Systemic) |
May elevate CYP3A4 substrates' serum concentration (High risk with Inhibitors). |
|
Idelalisib |
May elevate CYP3A4 substrates' serum concentration (High risk with Inhibitors). |
|
Ivabradine |
Ivabradine's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
Ivabradine |
The bradycardic effect of ivabradine may be enhanced by calcium channel blockers (nonhydropyridine). Ivabradine may increase Calcium Channel Blockers' ability to extend QTc (Nondihydropyridine). Particularly, bepridil's QTc prolonging effects might be improved. The serum levels of Ivabradine may rise in response to calcium channel blockers (Nondihydropyridine). Particularly, serum ivabradine concentrations may rise in response to verapamil or diltiazem. |
|
Lomitapide |
Lomitapide's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Naloxegol |
Naloxegol's serum levels may rise in response to moderately potent CYP3A4 inhibitors. |
|
Neratinib |
Neratinib's serum levels may rise in response to moderate CYP3A4 inhibitors. |
|
PAZOPanib |
The serum concentration of PAZOPanib may rise in response to P-glycoprotein/ABCB1 inhibitors. |
|
Pimozide |
Pimozide's serum levels may rise after taking CYP3A4 Inhibitors (Moderate). |
|
Simeprevir |
Simeprevir's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). |
|
Topotecan |
The serum concentration of topotecan may rise in response to P-glycoprotein/ABCB1 inhibitors. |
|
Ulipristal |
Ulipristal's serum levels may rise when taken with CYP3A4 Inhibitors (Moderate). Treatment: This is specific to the use of ulipristal for indications or symptoms of uterine fibroids (Canadian indication). When ulipristal is administered to patients as an emergency contraception, they should be watched closely for ulipristal toxicity. |
|
VinCRIStine (Liposomal |
The serum concentration of VinCRIStine may rise in response to P-glycoprotein/ABCB1 Inhibitors (Liposomal). |
Monitor:
- Blood Pressure and Heart Rate:
- Monitor regularly, especially in patients with renal and/or hepatic impairment.
- Liver Function Tests:
- Periodic tests to assess liver health.
- ECG:
- Consider periodic ECG monitoring, particularly in patients with renal and/or hepatic impairment.
Hypertension Guidelines:
- ACC/AHA 2017 Guideline:
- Confirmed hypertension with known cardiovascular disease (CVD) or high ASCVD risk: Target BP <130/80 mm Hg.
- Confirmed hypertension without increased ASCVD risk markers: Target BP <130/80 mm Hg may be reasonable.
- ADA 2019 Guidelines for Diabetes and Hypertension:
- Patients 18 to 65 years old, without ASCVD and <15% ASCVD risk: Target BP <140/90 mm Hg.
- Patients 18 to 65 years old with ASCVD or >15% ASCVD risk: Target BP <130/80 mm Hg may be appropriate if safe.
- Patients >65 years old (healthy or complex/intermediate health): Target BP <140/90 mm Hg.
- Patients >65 years old (very complex/poor health): Target BP <150/90 mm Hg.
How to administer Verapamil (Isoptin)?
Oral Administration:
- Do not crush or chew extended-release products.
Specific Instructions for Certain Products:
- Calan SR, Isoptin SR (Canadian product):
- Administer with food.
- Isoptin SR 240 mg tablet may be split in half.
- Verelan, Verelan PM:
- Capsules may be opened and contents sprinkled on 1 tablespoonful of applesauce.
- Swallow immediately (without chewing) and follow with a glass of cool water.
- Do not subdivide contents of capsules.
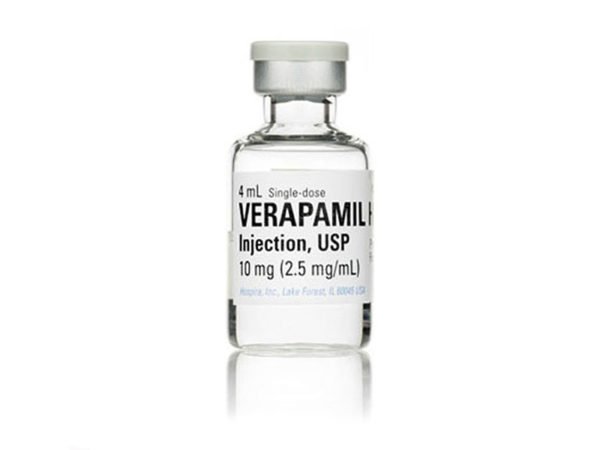
Intravenous (IV) Administration:
- Administer over at least 2 minutes.
- For older patients in the acute treatment of SVT, consider administering over 3 minutes according to ACLS guidelines.
Mechanism of action of Verapamil (Isoptin):
- Inhibits calcium ion entry into "slow channels" or specific voltage-sensitive areas of vascular smooth muscle and heart muscle cells during depolarization.
- Results in relaxation of coronary vascular smooth muscle and dilation of coronary arteries.
- Increases delivery of oxygen to the heart muscle in patients with vasospastic angina.
- Slows down the automaticity and conduction of the atrioventricular (AV) node, affecting heart rate and rhythm.
Note:
- Verapamil pharmacokinetics are influenced inversely by lean body weight.
Onset of Action and Peak Effect:
- Oral:
- Immediate Release: Onset 1 to 2 hours; Peak effect within 1 to 2 hours (Singh 1978).
- IV Bolus: Onset 3 to 5 minutes.
Duration:
- Oral:
- Immediate Release Tablets: Lasts 6 to 8 hours.
- IV: Lasts 0.5 to 6 hours (Marik 2011).
Absorption:
- Well, absorbed orally (>90%).
Distribution:
- Volume of distribution: 3.89 L/kg (Storstein 1984).
Protein Binding:
- Approximately 90%.
Metabolism:
- Metabolized in the liver with extensive first-pass effect via multiple CYP isoenzymes.
- Primary metabolite: Norverapamil (around 20% of verapamil's activity).
Bioavailability:
- Oral: 20% to 35%.
Half-life Elimination:
- Injection:
- Terminal half-life: 2 to 5 hours.
- Oral:
- Immediate Release:
- Single dose: 2.8 to 7.4 hours.
- Multiple doses: 4.5 to 12 hours.
- Extended Release: Approximately 12 hours.
- Severe Hepatic Impairment: 14 to 16 hours.
- Immediate Release:
Time to Peak Serum Level:
- Oral:
- Immediate Release: 1 to 2 hours.
- Extended Release:
- Calan SR: 5.21 hours.
- Verelan: 7 to 9 hours.
- Verelan PM: Around 11 hours (drug release delayed by about 4 to 5 hours).
Excretion:
- Primarily via urine (around 70% as metabolites, 3% to 4% as unchanged drug) and feces (at least 16%).
International Brands of Verapamil:
- APO-Verap
- APO-Verap SR
- DOM-Verapamil SR
- Isoptin SR
- MYLAN-Verapamil
- MYLAN-Verapamil SR
- NOVO-Veramil SR
- NOVO-Veramil
- PHL-VERAPAMIL SR
- PMS-Verapamil SR
- PRO-Verapamil SR
- RIVA-Verapamil SR
- Verelan
- Angimil
- Anpec
- Beaptin SR
- Calan SR
- Calaptin
- Cardiolen
- Cardiomil
- Caveril
- Cordilat
- Cordilox SR
- Cronovera
- Devincil
- Dilacoran
- Dilacoran Retard
- Fibrocard
- Flamon
- Hexasoptin
- Hypover
- Ikacor
- Ikapress
- Isoptin
- Isoptin Retard
- Isoptin RR
- Isoptin SR
- Isoptine
- Isoptino
- Lekoptin
- Lexoptin
- Librapamil
- Manidon
- Manidon Retard
- Quasar
- Securon
- Vasolan
- Vasomil
- Vasopten
- Vepiltax
- Verahexal
- Verahexal 240SR
- Veraloc
- Veramet
- Veramex
- Veramil
- Verap
- Verapamil Hydrochloride
- Verapamil Pharmavit
- Verapil
- Verapress 240 SR
- Verapress MR
- Veratad
- Veratens
- Verelan
- Vermine
- Verpamil
- Vetrimil
- Zolvera
Verapamil (Isoptin) Brands in Pakistan:
|
Verapamil (Hcl) [Inj 10 Mg/Ml] |
|
|
Canocil |
Pharmedic (Pvt) Ltd. |
|
Verapamil (Hcl) [Inj 50 Mg/Ml] |
|
|
Canocil |
Pharmedic (Pvt) Ltd. |
|
Verapamil (Hcl) [Inj 2.5 Mg/Ml] |
|
|
Isoptin |
Abbott Laboratories (Pakistan) Limited. |
|
Verapamil (Hcl) [Tabs 40 Mg] |
|
|
Calan |
Searle Pakistan (Pvt.) Ltd. |
|
Geopress |
Geofman Pharmaceuticals |
|
Isoptin |
Abbott Laboratories (Pakistan) Limited. |
|
Zavera |
Zafa Pharmaceutical Laboratories (Pvt) Ltd. |
|
Zeyar |
Zephyr Pharmatec (Pvt) Ltd. |
|
Verapamil (Hcl) [Tabs 80 Mg] |
|
|
Calan |
Searle Pakistan (Pvt.) Ltd. |
|
Geopress |
Geofman Pharmaceuticals |
|
Isocardin |
Pharmedic (Pvt) Ltd. |
|
Isoptin |
Abbott Laboratories (Pakistan) Limited. |
|
Veramil |
Caraway Pharmaceuticals |
|
Veramil |
Caraway Pharmaceuticals |
|
Zeyar |
Zephyr Pharmatec (Pvt) Ltd. |
|
Verapamil (Hcl) [Tabs 240 Mg] |
|
|
Geopress |
Geofman Pharmaceuticals |
|
Verapamil (Hcl) [Tabs Sr 240 Mg] |
|
|
Isoptin |
Abbott Laboratories (Pakistan) Limited. |
|
Zavera |
Zafa Pharmaceutical Laboratories (Pvt) Ltd. |
|
Verapamil (Hcl) [Caps Sr 240 Mg] |
|
|
Calan |
Searle Pakistan (Pvt.) Ltd. |


 for multiple myeloma.webp)
.jpg)