Asthma Severity Assessment includes three basic components:
- Symptoms control and Future risk of adverse outcomes
- Treatment-related issues, particularly treatment adherence and inhaler technique
- Comorbid conditions could add to the disease burden and affects the quality of life.
Lung Function tests, FEV-1 in particular, are an essential component of asthma severity assessment. Asthma Control is assessed by assessing the "symptomatic relief" and the "future risk of adverse outcomes".
It is best assessed with pre-designed questionnaires and lung function tests. Asthma Control is assessed before treatment initiation, at 3 - 6 months after treatment initiation to predict the personal best readings, and periodically thereafter to assess ongoing asthma control.
Asthma Severity Assessment in individuals older than 5 years of age:
Assess Asthma Control – Symptoms control and Future Risk |
|
Assess treatment Issues |
|
Assess Comorbidities |
Assess for comorbidities that can affect the patient's quality of life and affect treatment adherence and control:
|
How to Assess Asthma Symptoms Control?
Asthma symptom control should be assessed at each visit and during routine prescribing and dispensing of medications. Different patients may have different responses when they are asked about their asthma control.
Young individuals and athletes may experience more symptoms than elderly patients or those with a sedentary lifestyle. The four cardinal symptoms of asthma are:
- Cough
- Wheezing
- Shortness of breath
- Chest tightness or chest heaviness
Patients may report a combination of the above symptoms. Some symptoms may be more bothersome than others. It is important to identify the most troublesome symptoms and address those. All patients should be asked about the following symptoms during the last four weeks:
- The frequency of asthma symptoms (the number of symptomatic days per week)
- Frequency of night-waking due to symptoms or limitation of activity
- The frequency of short-acting beta-agonist (reliever medicines).
The use of SABA before exercise, ICS, or formoterol should not be included in the assessment of asthma control.
Asthma Symptoms Control Assessment Tools:
Different tools are being used to assess asthma symptoms control in children and adults.
Simple Screening Tools:
These tools can be used to rapidly identify those patients who need a more detailed assessment. One such tool is the "Consensus-based GINA symptom Control Tool". This correlates with the numerical asthma assessment control tools.
GINA assessment of Asthma Control:
Asthma Symptoms Control |
Level of Asthma symptoms Control |
|||
| In the past four weeks, has the patient had: | Well-controlled | Partly Controlled | Uncontrolled | |
| Day time symptoms more than twice a week |
|
None of these symptoms | 1 – 2 of these symptoms | 3 – 4 of these symptoms |
| Night waking due to asthma |
|
|||
| SABA-reliever use for more than twice a week |
|
|||
| Any activity limitation due to Asthma |
|
|||
The Asthma symptoms Control assessment tool is usually combined with asthma risk assessment. Asthma risk factors should be assessed at the time of diagnosis and periodically thereafter.
FEV-1 should be measured at the start of the treatment, at 3 - 6 months of controller treatment to assess the personal best, and 1 - 2 yearly thereafter or as clinically indicated, especially in patients experiencing exacerbations.
Risk Factors for Poor Asthma Outcomes:
|
Any of the following risk factors increase the patient's risk factors for asthma exacerbation even if few asthma symptoms are present: An important risk factor for asthma exacerbation is uncontrolled asthma symptoms. Additional modifiable risk factors for asthma flares (even without symptoms) include:
|
|
Risk factors for developing persistent airflow limitation:
|
|
Risk Factors for medication Side effects:
|
Other examples of asthma symptoms control tools are:
Simplified PACS tool (Primary care Asthma Control Screening tool) [Ref]: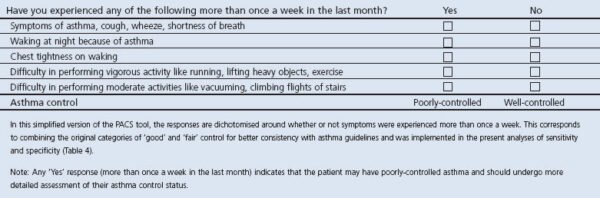
The 30 seconds asthma test:

Categorical symptoms Control Tools:
These include: The Royal College of Physician 3 Question Tool:  The Patient Asthma APGAR Score can be downloaded here as PDF: Download
The Patient Asthma APGAR Score can be downloaded here as PDF: Download
Assessing the future risk of adverse outcomes:
Assessing future risk is the next important component of asthma severity assessment. This includes identifying whether the patient is at risk of exacerbations, persistent airflow limitation, and adverse medication side effects.
Asthma symptoms are a strong predictor of adverse outcomes, however, they should not be used alone for predicting future risk assessment because:
- Asthma symptoms can be controlled by inappropriate and excessive use of LABA.
- Respiratory symptoms may be due to lack of fitness, comorbid conditions, or inducible laryngeal obstruction.
- Some patients may have low lung function but fewer symptoms
- Anxiety may contribute to symptoms.
Risk Factors for Exacerbations:
The most important risk factor for asthma exacerbation is poor asthma symptom control, however, additional risk factors also play an important role. The risk factors for asthma exacerbations are summarized in the table below:
|
Any of the following risk factors increase the patient's risk factors for asthma exacerbation even if few asthma symptoms are present. An important risk factor for asthma exacerbation is uncontrolled asthma symptoms. |
|
| Additional modifiable risk factors for asthma flares (even without symptoms) include: | |
| Medications: | High SABA use (exceeding 1 x 200 mcg – dose canister/month) |
| Inadequate ICS: | Poor adherence, inaccurate inhaler technique, not prescribed ICS |
| Comorbidities: |
|
| Exposures: |
|
| Context: |
|
| Lung function: |
|
| Other Tests in patients with Type 2 inflammation: |
|
| Other major independent risk factors for flare-ups include: |
|
Risk Factors for the development of persistent airflow limitation:
Lung function declines by 15 - 20 ml per year. In asthmatics, the rate of decline may be more rapid. A decline in lung function may be associated with more persistent shortness of breath and asthma symptoms.
Children with persistent airflow limitation may have reduced growth and an accelerated decline in lung functions during adulthood. Factors leading to persistent airflow limitation are summarized in the table below:
Risk factors for developing persistent airflow limitation: |
|
| History: |
|
| Medication: |
|
| Exposures: |
|
| Investigations: |
|
Risk Factors for medication side effects:
Medication side effects that are important are usually caused by the frequent use of systemic corticosteroids, long-term and potent inhaled corticosteroids use, and local effects caused by an incorrect inhaler technique.
The risk of corticosteroid-induced osteoporosis, cataract formation, diabetes, hypertension, and hypothalamic adrenal suppression is increased with the long-term use of potent inhaled corticosteroids or systemic corticosteroids. Local adverse medication side effects include oral thrush and dysphonia.
Risk Factors for medication Side effects: |
|
| Systemic: |
|
| Local: |
|
Role of Lung Function in assessing Asthma Control:
Relation between lung function and asthma control measures:
A low FEV-1 is considered a strong and independent predictor of asthma exacerbation. However, it does not correlate well with asthma symptoms control in adults and children.
Lung function should be assessed before treatment initiation, at 3 - 6 months of controller treatment to predict the personal best, and every one or two years thereafter or as clinically indicated.
Lung function should be more frequently performed in patients at risk of exacerbation such as those with persistent and severe asthma. For individuals who have a confirmed diagnosis of asthma and whose asthma is relatively controlled, treatment should not be generally stopped prior to the visit.
Interpretation of lung function tests in patients with Asthma:
- A low predicted FEV-1 percent:
- It is a predictor of asthma exacerbations, independent of asthma symptoms particularly if the FEV-1 is less than 60%.
- A low FEV-1 is a predictor of a long-term decline in lung function, independent of symptoms.
- Patients who do not report symptoms despite a low FEV-1 may have persistent airway inflammation. It may be suggestive of a poor perception of the airflow limitation and limitation in the lifestyle.
- A normal or near-normal FEV-1 in the symptomatic patient:
- Normal lung functions in a symptomatic patient should prompt the investigation of other diseases.
- These patients should be investigated for diseases such as cardiac diseases, post-nasal drip, gastroesophageal reflux disease, or inducible laryngeal obstruction.
- Persistent bronchodilator reversibility:
- Persistent bronchodilator reversibility is the improvement in the FEV-1 by 12% or 200 ml from the baseline despite the use of SABA within the previous four hours or LABA within 12 hours.
- It is indicative of poor and uncontrolled asthma.
Interpretation of changes in lung function tests in clinical practice:
With the regular use of ICS treatment, the FEV-1 starts to improve within days and reaches a plateau in about two months. At 2 to 6 months, lung function tests should be repeated to predict the personal best value that can be used for future reference.
Despite using ICS, some patients may have a faster decline in lung function. These patients may be given a trial of high-dose inhaled corticosteroids or a short course of systemic corticosteroids. If no improvement is noted, high-dose corticosteroids should not be used for a prolonged period of time.
The role of short-term and long-term PEF monitoring:
PEF (Peak expiratory flow rate) monitoring is done once the diagnosis is established to assess the response to the treatment, evaluate the triggers for worsening asthma symptoms, and develop a baseline asthma action plan.
PEF reading improves within days of initiating inhaled corticosteroids and reaches a personal best within two weeks. The average PEF continues to decrease for about three months along with a reduction in the diurnal variation.
Excessive diurnal variability is suggestive of poor asthma control and an increased risk of asthma exacerbations. Peak flow monitoring is now only recommended for patients with a poor perception of airflow limitation and those with severe asthma.
Asthma Severity Assessment in Clinical Practice:
The asthma severity assessment is done retrospectively by the level of treatment required for the patient and the risk of exacerbations. Asthma severity is not a static value and changes over time.
It is best recorded once the patient is on treatment for several months and appropriate treatment step-down has been attempted to find the patient's minimum effective treatment. It is classified as:
Mild Asthma:
- Mild asthma is one that is controlled at step 1 or step 2 of the asthma management plan.
- It is controlled with ICS-formoterol alone or with a maintenance controller treatment such as a low dose ICS, leukotriene receptor inhibitor, or chromones.
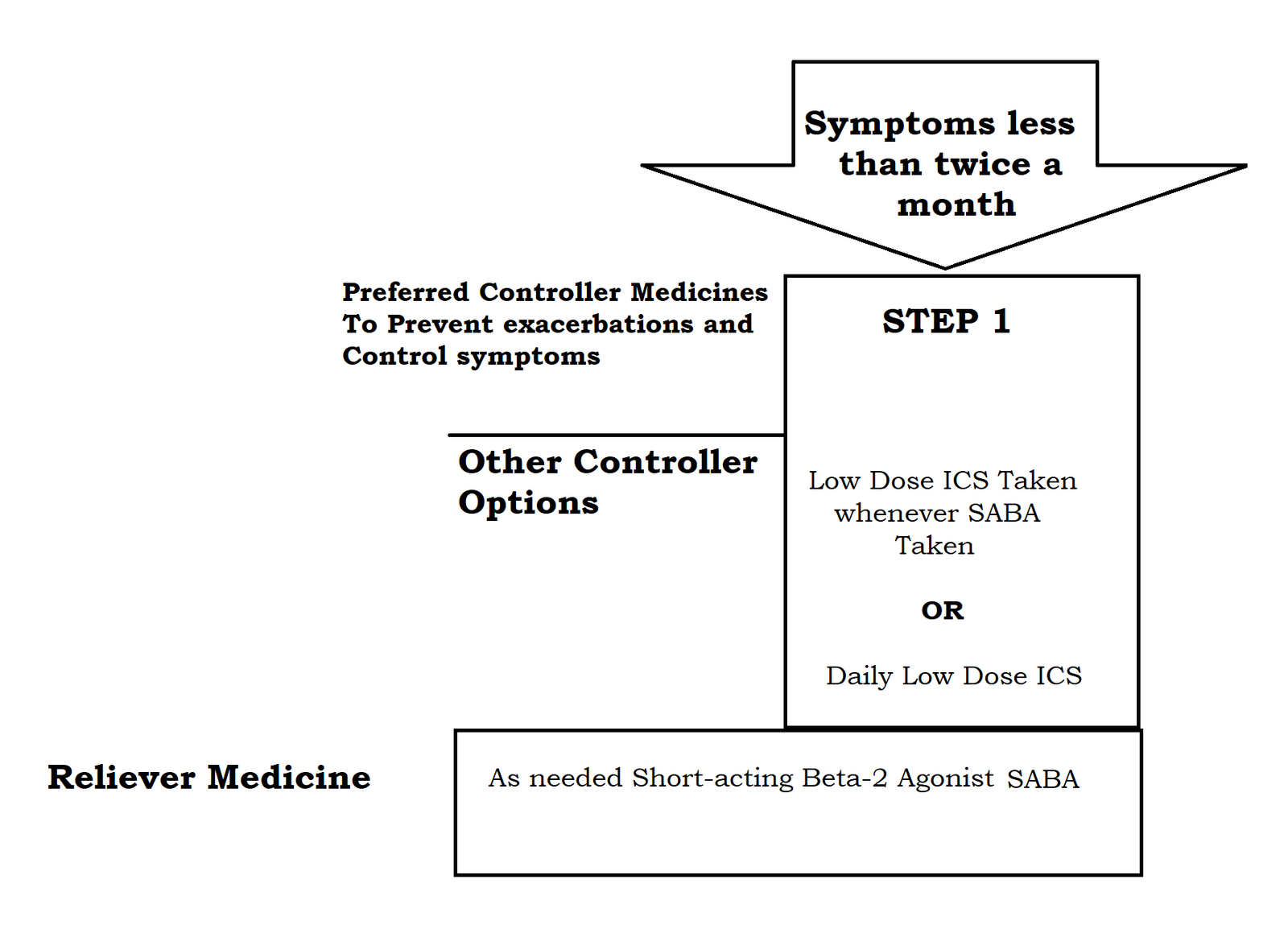 Step one (Mild) Asthma management
Step one (Mild) Asthma management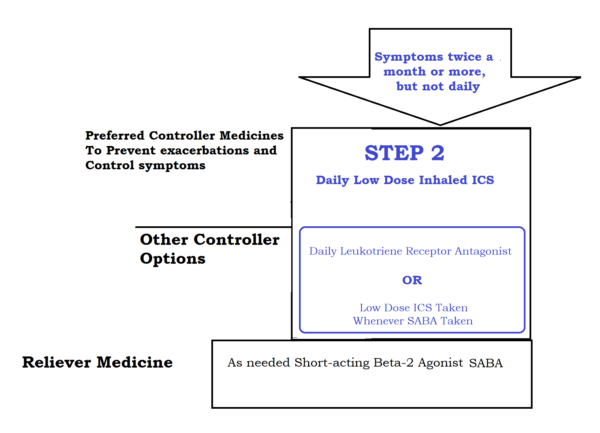 Step 2 (mild) asthma treatment
Step 2 (mild) asthma treatment
Moderate Asthma:
- Moderate asthma is the one that is controlled at step 3 of the treatment plan i.e. ICS-LABA
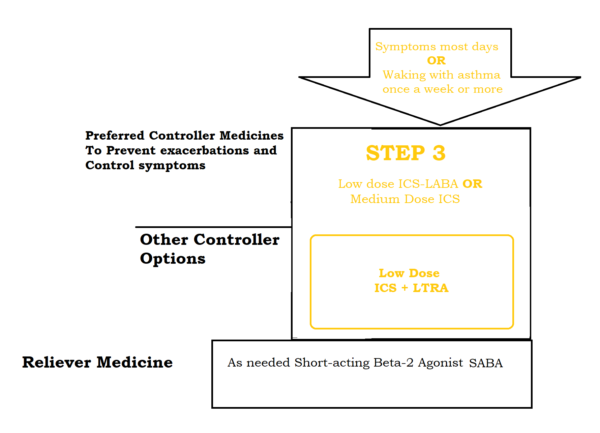 Step 3 (moderate) asthma treatment
Step 3 (moderate) asthma treatment
Severe Asthma:
- Severe asthma requires steps 4 and above of the treatment.
- Patients require high-dose ICS to control the disease, or it remains uncontrolled despite high-dose ICS.
- Most of these patients are not adherent to the prescribed treatment or have a faulty inhaler technique.
- Many patients have comorbid conditions that are not well taken care of resulting in persistent symptoms and airflow limitation. These may include heart diseases, GERD, Obesity, and chronic rhinosinusitis.
 Steps 4 and 5 asthma (severe asthma) management
Steps 4 and 5 asthma (severe asthma) management
Problems to look into before making the diagnosis of severe asthma:
- Inhaler technique (up to 80% of the patients with severe and controlled asthma have a poor inhaler technique)
- Poor adherence to the drugs
- Comorbid conditions such as obesity, rhinosinusitis, obstructive sleep apnea, and cardiac failure
- Incorrect diagnosis
- Continuous exposure to a sensitizing agent.
In Conclusion:
Asthma Severity assessment is a dynamic process and the severity may change with medications, allergen exposure, and comorbid conditions. It should be done before deciding on the treatment.






