Atropine is a medication and a naturally occurring alkaloid derived from plants of the Solanaceae family, including deadly nightshade (Atropa belladonna), Jimson weed (Datura stramonium), and others. It has a variety of uses in medicine, primarily based on its ability to act as an anticholinergic agent, meaning it blocks the action of the neurotransmitter acetylcholine in the nervous system.
Acetylcholine's function at parasympathetic locations in the central nervous system, secretory glands, and smooth muscle is blocked by atropine.
It is used in the therapy of the following conditions:
- Atropine use as an Antidote:
- In order to decrease the negative effects of anticholinesterases (such as edrophonium and neostigmine) during the restoration of neuromuscular blockade, it is also used in conjunction with them.
- The main application is as a remedy for anticholinesterase poisoning (carbamate insecticides, nerve agents, organophosphate insecticides)
- It serves as a remedy for poisoning brought on by muscarine-containing mushrooms.
- Atropine use in Cardiovascular conditions:
- Atrioventricular (AV) nodal block and symptomatic sinus bradycardia are both treated with it.
- The treatment of asystole or pulseless electrical activity no longer calls for its usage.
- For type II second-degree or third-degree AV block, it could not be effective.
- Atropine use in Respiratory tract medicine:
- It is often used as a preoperative or anaesthetic drug to reduce secretions and salivation.
- Off-Label Usage of Atropine In Adults:
- Premedication in rapid sequence intubation.
- It is also used as an adjunct chronotropic agent in stress echocardiography.
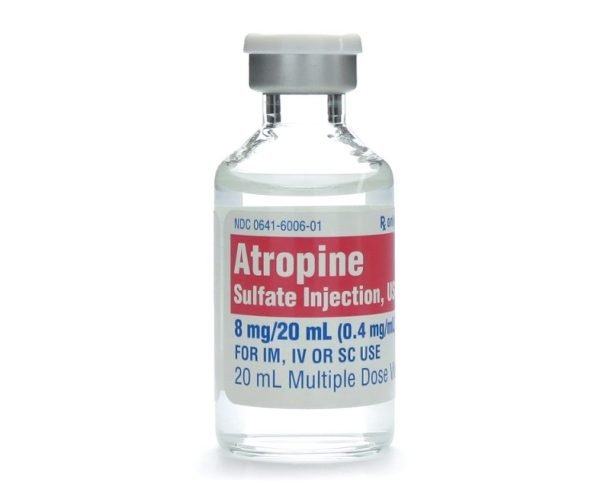
Atropine Dose in Adults
It's important to use atropine carefully because if given in doses less than 0.5 mg through an IV, it can unexpectedly cause the heart rate to slow down instead of speeding up. Also, when treating patients with heart disease, the total amount of atropine given should be limited to 0.03 to 0.04 mg per kg of the person's body weight to avoid further heart complications.
Atropine Dosage for excessive salivation and secretions (preanesthesia):
- It is administered either intramuscularly (IM), intravenously (IV), or subcutaneously (SubQ).
- The typical dose is 0.4 to 1 mg given 30 to 60 minutes before the operation.
- This dose can be repeated every 4 to 6 hours as needed, but the total dose should not exceed 3 mg.
- This precaution helps manage secretions effectively during surgery while minimizing potential side effects and complications.
Atropine Dose in the treatment of Bradycardia:
- It can be administered intravenously (IV) or intramuscularly (IM) at a dose of 0.5 mg every 3 to 5 minutes as needed, with a maximum total dose of 3 mg.
- There is also an option to administer atropine endotracheally (directly into the trachea) for cases where IV or IM administration is not possible, at a dose of 1 to 2 mg every 3 to 5 minutes.
Note:
- It's important to note that atropine may not be effective in patients who have had a heart transplant, as these patients often lack the normal nerve connections (vagal innervation) that atropine targets to increase heart rate.
Atropine off-label atropine Dose in the treatment of Muscarine-containing mushroom poisoning:
- In cases of muscarine poisoning, atropine can be administered intravenously (IV) in doses of 1 to 2 mg.
- The dosage may be adjusted and repeated as necessary based on the patient's response to the treatment.
Atropine Dose in the treatment of Neuromuscular blockade reversal:
- When combined with neostigmine, the recommended dose of atropine is 15 to 30 micrograms per kilogram (mcg/kg), administered intravenously (IV).
- If used with edrophonium, the atropine dose is slightly lower, ranging from 7 to 10 mcg/kg.
- These combinations are used to counteract the effects of muscle relaxants, allowing normal muscle function to resume more quickly and safely after surgical procedures.
Atropine dosage for treating poisoning from organophosphate, carbamate, pesticide, or nerve agent:
Atropine for Insecticide or Nerve Agent Poisoning
Overview
- Atropine is used to treat poisoning caused by organophosphate or carbamate insecticides or nerve agents.
- Dosage varies depending on poisoning severity, with greater amounts typically required for nerve agents.
- Patients may need higher doses due to tolerance, especially in severe cases.
Administration
- Initial Dose: 1 to 6 mg, given intravenously (IV), intramuscularly (IM), or via endotracheal tube.
- Repeat Doses: Every 3 to 5 minutes, doubling the dose if no response. Continue for 2 to 12 hours as symptoms recur.
- AtroPen (IM):
- Mild Symptoms: Administer 2 mg immediately, with up to 2 additional doses if severe symptoms develop.
- Severe Symptoms: Administer three 2 mg doses rapidly.
- Symptoms of Poisoning:
- Mild: Blurred vision, bradycardia, breathing difficulties, drooling, nausea, etc.
- Severe: Severe breathing difficulties, seizures, unconsciousness, etc.
IV Infusion
- Administer 10% to 20% of the total loading dose required via continuous IV infusion per hour.
- Adjust as needed to maintain response without causing atropine toxicity.
Atropine off-label atropine Dose in the Rapid sequence intubation (premedication):
- It's given intravenously (IV) at a dose of 0.01 to 0.02 milligrams per kilogram (mg/kg) of body weight.
- The smallest dose given is 0.1 mg, and the largest single dose shouldn't exceed 0.5 mg.
- This helps prepare the patient's body for intubation by reducing saliva and other secretions in the airway, making the procedure smoother and safer.
Atropine off label atropine Dose in the treatment of Stress echocardiography (adjunct chronotropic agent):
- It's given intravenously (IV) at a dose of 0.25 to 0.5 milligrams (mg), up to a total dose of 1 to 2 mg, until the heart reaches 85% of its target rate.
- This helps increase the heart rate, allowing for better assessment of heart function during the test.
Atropine Dose in Children
Atropine Dose in the treatment of Bradycardia:
Atropine for Bradycardia in Infants, Children, and Adolescents
- Atropine is used to treat bradycardia (slow heart rate) in pediatric patients.
- Dosage varies based on the child's weight and route of administration.
Intravenous (IV) or Intraosseous Administration
- Dosage: 0.02 milligrams per kilogram (mg/kg) per dose.
- Minimum Dose: 0.1 mg per dose.
- Maximum Dose: 0.5 mg per dose.
- Repeat: May be repeated once every 5 minutes if necessary.
- Usage: Reserved for patients who do not respond to improved oxygenation and epinephrine.
- Note: Some recommend avoiding the minimum dose in patients weighing less than 5 kilograms.
Endotracheal Administration
- Dosage: 0.04 to 0.06 mg/kg per dose.
- Repeat: May be repeated once if necessary.
Atropine Dosage in the treatment to Inhibit salivation and secretions (preoperative/ intraoperative):
Infants and Children <12 years
- Dosage: 0.02 milligrams per kilogram (mg/kg) per dose.
- Maximum Dose: 0.5 mg per dose.
- Administer: First dose 30 to 60 minutes before surgery, then repeat every 4 to 6 hours as needed.
- Maximum Total Dose: 1 mg per procedure.
Children ≥12 years and Adolescents
- Dosage: 0.02 mg/kg per dose.
- Maximum Dose: 1 mg per dose.
- Administer: First dose 30 to 60 minutes before surgery, then repeat every 4 to 6 hours as needed.
- Maximum Total Dose: 2 mg per procedure.
Atropine Premedication Dose in the emergency Intubation:
- Atropine may be considered in high-risk situations for bradycardia during intubation in infants and children.
- Routine use is not recommended unless there is a high risk of bradycardia, such as when using succinylcholine or in septic shock.
Infants and Children
- Dosage: 0.02 milligrams per kilogram (mg/kg) per dose.
- No Minimum Dose: There is no specified minimum dose.
- Maximum Dose: 0.5 mg per dose.
- Administration: Given intravenously (IV) before intubation.
- Usage: Reserved for situations with a high risk of bradycardia, such as when using succinylcholine or in septic shock.
Atropine Dose in the treatment of Muscarine-containing mushroom poisoning:
- Atropine may be used in the treatment of poisoning caused by muscarine-containing mushrooms.
- Data on its use in this context are limited.
Infants, Children, and Adolescents
- Dosage: 0.02 milligrams per kilogram (mg/kg) per dose.
- Minimum Dose: 0.1 mg.
- Administration: Intravenous (IV).
- Repeat: Titrate and repeat doses as needed based on the patient's response.
- Note: Due to limited data, careful monitoring and individualized dosing are essential in treating muscarine-containing mushroom poisoning with atropine.
Atropine Dose in the treatment of Organophosphate or carbamate insecticide or nerve agent poisoning:
- Atropine is a critical component of the treatment for poisoning caused by organophosphate or carbamate insecticides or nerve agents.
- Antidotal therapy should be administered promptly upon the appearance of symptoms, without waiting for confirmation of exposure.
Dosage and Administration
IV, IM, Intraosseous:
- Infants and Children: Initial dose of 0.05 to 0.1 milligrams per kilogram (mg/kg). Repeat every 5 to 10 minutes as needed, doubling the dose if previous dose does not induce atropinization.
- Adolescents: Initial dose of 1 to 3 mg/dose. Repeat every 3 to 5 minutes as needed, doubling the dose if previous dose does not induce atropinization.
- Continuous IV Infusion: Following atropinization, administer 10% to 20% of the total loading dose required as a continuous IV infusion per hour.
IM (AtroPen):
- Dosage depends on symptom severity and patient's weight.
- Mild Symptoms: Administer weight-directed dose as soon as exposure is known or suspected. Repeat doses may be given if severe symptoms develop.
- Severe Symptoms: Immediately administer three weight-directed doses in rapid succession.
Endotracheal:
- Increase the dose by 2 to 3 times the usual IV dose.
- Mix with normal saline and administer. Flush with normal saline and follow with assisted manual ventilations.
Monitoring and Considerations
- Titrating atropine to pulmonary status (decreased bronchial secretions) is important.
- Consider continuous IV infusion in patients requiring large doses of atropine.
- Pralidoxime is also a component of the management; refer to specific guidelines for its administration.
Atropine Pregnancy Risk Factor B/C
- Atropine is classified as Pregnancy Risk Factor B/C, meaning there is limited data on its safety during pregnancy.
- While animal studies didn't show adverse effects, atropine does cross the human placenta.
- However, in emergencies like cardiac arrest during pregnancy, medications including atropine are used as in non-pregnant women following standard guidelines.
- Administering antidotes like atropine to pregnant women should be based on the mother's health needs; they shouldn't be withheld due to concerns about fetal harm.
- It's important to follow Advanced Cardiovascular Life Support guidelines for dosage and indications, prioritizing the mother's health while considering potential risks to the fetus.
Atropine use during breastfeeding:
- Atropine is detected in small amounts in breast milk, and its effects on breastfeeding infants are uncertain, with conflicting data.
- There's a possibility that atropine might reduce milk production or lead to adverse effects in the nursing baby.
- Therefore, caution is advised when considering the use of atropine in breastfeeding women.
- It's essential to weigh the potential benefits against possible risks and consult with a healthcare provider before taking atropine while breastfeeding.
Atropine dose in kidney disease:
- The manufacturer's labeling for atropine does not specify any dosage adjustments for patient with kidney disease.
Atropine dose in liver disease:
- The manufacturer's labeling for atropine does not specify any dosage adjustments for patient with liver disease.
Side effects of atropine:
- Cardiovascular:
- Bradycardia
- Chest Pain
- Atrioventricular Dissociation (Transient)
- Bigeminy
- Asystole
- Atrial Arrhythmia
- Atrial Fibrillation
- Decreased Blood Pressure
- R On T Phenomenon
- Shortened RT Duration
- Prolonged QT Interval
- ECG Changes (Prolonged P Wave
- Shortened PR Segment
- Widening Of QRS Complex
- Ectopic Beats (Atrial)
- Supraventricular)
- Flushing
- Increased Blood Pressure
- Flattened T Wave
- Repolarization Abnormalities
- ST-Segment Elevation
- Retrograde Conduction)
- Left Heart Failure
- Myocardial Infarction
- Nodal Arrhythmia (No P Wave On ECG)
- Palpitations
- Extrasystoles (Nodal
- Ventricular Fibrillation
- Ventricular Flutter
- Ventricular Premature Contractions
- Ventricular Tachycardia
- Tachycardia
- Trigeminy
- Ventricular Arrhythmia (Including Flutter)
- Weak Pulse (Or Impalpable Peripheral Pulses)
- Ventricular
- Sinus Tachycardia
- Supraventricular Tachycardia (Including Junctional Tachycardia)
- Central Nervous System:
- And Signs Of Drowsiness)
- Agitation (Children)
- Amnesia
- Anxiety
- Dysmetria
- Emotional Disturbance
- Restlessness
- Seizure (Generally Tonic-Clonic)
- Stupor
- Vertigo
- Abnormal Electroencephalogram (Runs Of Alpha Waves
- Increase In Photic Stimulation
- Ataxia
- Behavioral Changes
- Coma
- Confusion
- Decreased Deep Tendon Reflex
- Irritability (Children)
- Lack Of Concentration
- Lethargy (Children)
- Delirium
- Excitement
- Feeling Hot
- Hallucination (Visual Or Aural)
- Headache
- Hyperpyrexia
- Dizziness
- Drowsiness
- Dysarthria
- Hyperreflexia
- Hypertonia
- Insomnia
- Intoxicated Feeling
- Mania
- Myoclonus
- Neurologic Abnormality
- Nocturnal Enuresis
- Opisthotonus
- Paranoia
- Positive Babinski Sign
- Dermatologic:
- Dry And Hot Skin
- Maculopapular Rash
- Papular Rash
- Anhidrosis
- Cold Skin
- Dermatitis
- Scarlatiniform Rash
- Erythematous Rash
- Hyperhidrosis
- Macular Eruption
- Skin Rash
- Endocrine & Metabolic:
- Dehydration
- Hyperglycemia
- Hypoglycemia
- Hypokalemia
- Hyponatremia
- Increased Thirst
- Loss Of Libido
- Neuromuscular & Skeletal:
- Laryngospasm
- Muscle Twitching
- Weakness
- Gastrointestinal:
- Delayed Gastric Emptying
- Diminished Bowel Sounds
- Malabsorption
- Nausea
- Abdominal And Bladder Distension
- Abdominal Pain
- Constipation
- Oral Lesion
- Paralytic Ileus
- Salivation
- Vomiting
- Dry Mucous Membranes
- Dysphagia
- Xerostomia
- Genitourinary:
- Urinary Hesitancy
- Urinary Retention
- Difficulty In Micturition
- Impotence
- Urinary Urgency
- Miscellaneous:
- Failure To Thrive
- Fever (Secondary To Decreased Sweat Gland Activity)
- Swelling (Children)
- Local:
- Injection Site Reaction
- Hematologic & Oncologic:
- Increased Hemoglobin
- Leukocytosis
- Abnormal Erythrocytes (Increased)
- Decreased Hemoglobin
- Petechiae
- Hypersensitivity:
- Hypersensitivity Reaction
- Ophthalmic:
- Abnormal Eye Movements (Cyclophoria And Heterophoria)
- Angle-Closure Glaucoma (Acute)
- Blepharitis
- Blindness
- Blurred Vision
- Conjunctivitis
- Crusted Of Eyelid
- Cycloplegia
- Decreased Accommodation
- Decreased Visual Acuity
- Dry Eye Syndrome
- Eye Irritation
- Keratoconjunctivitis Sicca
- Lacrimation
- Mydriasis
- Photophobia
- Strabismus
- Renal:
- Increased Blood Urea Nitrogen
- Respiratory:
- Bradypnea
- Changes In Respiration (Labored Respiration)
- Cyanosis
- Dyspnea
- Laryngitis
- Pulmonary Edema
- Respiratory Failure
- Stridor (Inspiratory)
- Tachypnea
Contraindications to Atropine:
- According to the manufacturer's labeling, there are no contraindications specified for the use of atropine.
Warnings and precaution
Anaphylaxis
- Anaphylaxis, a severe allergic reaction, is a potential risk associated with the use of atropine.
Arrhythmias:
- For certain heart rhythm problems like type II second-degree or third-degree AV block, it's best to avoid using atropine as the main treatment.
- Atropine may not be effective and could potentially worsen these conditions, especially if there's a new wide QRS complex.
- While using atropine for asystole (no heartbeat) or bradycardic pulseless electrical activity (PEA) hasn't been shown to cause significant harm, it's not likely to help either, according to updated guidelines.
- In these cases, other treatments are preferred for better outcomes.
Hyperthermia
- In hot environments, using atropine can lead to hyperthermia, a condition where the body overheats.
- This can cause heat prostration, where the body struggles to cool down and may result in symptoms like heavy sweating, weakness, and fainting.
Psychosis:
- In some cases, sensitive individuals or those who take too much atropine may experience psychosis, a mental condition characterized by a loss of touch with reality.
Autonomic neuropathy:
- Patients with autonomic neuropathy should use atropine with caution.
- Autonomic neuropathy affects the nerves that control involuntary bodily functions like heart rate, blood pressure, and digestion.
Gastrointestinal Disease:
- In patients with gastrointestinal disease, using atropine may lead to complications.
- It's important to note that atropine use can potentially worsen conditions like partial organic pyloric stenosis, turning it into complete obstruction.
- Additionally, atropine should be avoided in patients with paralytic ileus, intestinal atony (lack of muscle tone) in elderly or debilitated patients, severe ulcerative colitis, and toxic megacolon associated with ulcerative colitis.
- These conditions can be exacerbated by atropine, so it's crucial to use caution and consider alternative treatments in such cases.
Cardiovascular disease
- In patients with cardiovascular disease, including conditions like myocardial ischemia, heart failure, tachyarrhythmias (such as sinus tachycardia), and hypertension, atropine should be used cautiously.
- This is because atropine can cause increases in blood pressure and heart rate as part of its effects, which might worsen ischemia (reduced blood flow to the heart muscle), trigger a heart attack (MI), or increase the risk of arrhythmias (abnormal heart rhythms).
Glaucoma:
- Using atropine in individuals with glaucoma can precipitate acute glaucoma, a sudden increase in pressure within the eye.
Hepatic impairment
- In patients with hepatic impairment, caution is advised when using atropine because its effects may be prolonged, especially in cases of severe hepatic impairment.
Hiatal hernia
- In patients with hiatal hernia, particularly those with associated reflux esophagitis, caution should be exercised when using atropine.
Hyperthyroidism:
- In patients with hyperthyroidism, caution should be exercised when using atropine.
Myasthenia gravis:
- In individuals with myasthenia gravis, extreme caution should be exercised when considering the use of atropine, especially when it's intended to treat side effects of acetylcholinesterase inhibition or when possible, it should be avoided altogether.
Renal impairment
- In patients with renal impairment, caution is advised when using atropine because its effects may be prolonged, especially in cases of severe renal impairment.
Respiratory impairment
- In patients with respiratory impairment, using atropine can lead to the thickening of bronchial secretions and the formation of thick plugs, particularly in those with chronic lung disease.
Urinary retention
- In patients with conditions like prostatic hypertrophy, using atropine can potentially lead to complete urinary retention, where the bladder cannot empty properly.
- Additionally, in individuals with obstructive uropathy or other conditions causing urinary retention, atropine should be avoided, if possible, to prevent worsening of symptoms.
- Atropine works by relaxing certain muscles, including those in the bladder, which can interfere with normal urination in these patients.
Monitor:
- Heart Rate, Blood Pressure, Pulse, Mental Status: Regularly monitor these vital signs to ensure they remain within normal ranges and to assess the patient's overall condition.
Intravenous Administration
- Requires a Cardiac Monitor: When administering atropine intravenously, use a cardiac monitor to closely monitor the patient's heart rhythm and ensure their safety.
Organophosphate or Carbamate Insecticide or Nerve Agent Poisoning
- Heart Rate, Blood Pressure, Respiratory Status, Oxygenation, Secretions: Monitor these parameters closely, as they can be affected by poisoning. Maintain atropinization with repeated dosing as needed based on clinical status.
- Signs of Inadequate Dosing: Watch for crackles in lung bases or continuation of cholinergic signs, which may indicate that the dose of atropine is insufficient. Pulmonary improvement may not necessarily match other signs of atropinization.
Atropine Toxicity
- Monitor for Signs and Symptoms: Keep an eye out for signs of atropine toxicity, such as fever, muscle twitching, or confusion. If toxicity occurs, stop administering atropine and monitor the patient closely.
- Consult Institutional Policies: Follow individual institutional policies and procedures for the management of atropine administration and toxicity.
How to administer Atropine?
IM Administration (AtroPen)
- Injection Site: Administer to the outer thigh.
- Procedure: Firmly grasp the autoinjector with the appropriate colored tip (green or black) pointed down. Remove the safety release. Jab the tip at a 90° angle against the outer thigh, even through clothing if necessary. In thin patients, bunch up the thigh before injection. Hold in place for 10 seconds, then remove and massage the site. If the needle is not visible after use, repeat the process. Bend the needle after use to prevent injury.
IV Administration
- Method: Administer undiluted by rapid IV injection. Slow injection may lead to paradoxical bradycardia.
- Bradycardia: If bradycardia is present, do not delay treatment with external pacing.
Intraosseous (IO) Administration
- May administer intraosseous if needed.
Endotracheal Administration
- Dilution: Dilute in ≤10 mL NS or sterile water. Absorption may be greater with sterile water.
- Procedure: Stop compressions (if for cardiac arrest), then spray the drug quickly down the tube. Follow immediately with several quick insufflations and continue chest compressions.
SubQ Administration
- May administer subcutaneous if needed.
Mechanism of action of Atropine:
- Atropine works by blocking the action of acetylcholine at parasympathetic sites in smooth muscle, secretory glands, and the central nervous system.
- This action leads to increased cardiac output and drying of secretions.
- In cases of cholinergic poisoning caused by agents with acetylcholinesterase inhibitor activity, atropine acts as a competitive antagonist of acetylcholine at muscarinic receptors, reversing the muscarinic effects.
- Its primary goal in such poisonings is to reverse excessive mucus production and airway constriction.
- Importantly, atropine doesn't affect the nicotinic receptors responsible for muscle weakness, twitching, and paralysis associated with cholinergic poisoning.
The onset of action:
- Inhibition of Salivation (IM): Begins within 30 minutes; reaches maximum effect in 30 to 60 minutes.
- Increased Heart Rate (IM): Starts within 15 to 30 minutes; maximum effect seen in 45 to 60 minutes.
- Increased Heart Rate (IV): Immediate onset; maximum effect in 0.7 to 4 minutes.
Duration:
- Inhibition of Salivation (IM): Lasts up to 4 hours.
Absorption:
- Rapid and well absorbed from all dosage forms.
Distribution:
- Widely throughout the body, including crossing the blood-brain barrier.
Protein Binding:
- Ranges from 14% to 44%.
Metabolism:
- Occurs in the liver via enzymatic hydrolysis.
Half-life Elimination:
- Children under 2 years: 6.9 ± 3 hours.
- Children over 2 years: 2.5 ± 1.2 hours.
- Adults: 3 ± 0.9 hours.
- Elderly (65 to 75 years): 10 ± 7.3 hours.
Time to Peak:
- IM: 30 minutes.
- IM autoinjector: 3 minutes.
Excretion:
- Primarily via urine, with 13% to 50% excreted as unchanged drug and metabolites.
International Brands of Atropine:
- Nespin
- Atren
- Atro
- Atropa
- Atropan
- Atropin
- Atropin Biotika
- Atrosol
- Bellafit
- Bellafit N
- Cholspas Atropin
- Ciratro
- Dysurgal
- Endotropina
- Estropin
- Santropina
- Stellatropine
- Tropyn
Atropine brand names in Pakistan:
|
Atropine (Sulphate) Injection 1 Mg/Ml |
|
|
Atropine |
P.D.H. Pharmaceuticals (Pvt) Ltd. |
|
Atropine Sulphate |
Shifa Laboratories. (Pvt) Ltd. |
|
Elitopine |
Elite Pharma |
|
Atropine (Sulphate) Eye Drops 1 %W/V |
|
|
Atropine |
Lahore Chemical & Pharmaceutical Works (Pvt) Ltd |
|
Atropine |
Harmann Pharmaceutical Laboratories (Pvt) Ltd. |
|
Atropine Sulphate |
Shifa Laboratories. (Pvt) Ltd. |
|
Atropisole |
Lahore Chemical & Pharmaceutical Works (Pvt) Ltd |
|
Ethiatropine |
Ethical Laboratories (Pvt) Ltd. |
|
Eytropine |
Orient Laboratories |
|
Ophth-Atropine |
Ophth-Pharma (Pvt) Ltd. |
|
Opta Atropine |
Remington Pharmaceutical Industries (Pvt) Ltd. |
|
Optapine |
Harmann Pharmaceutical Laboratories (Pvt) Ltd. |
|
Orbatropin |
Zafa Pharmaceutical Laboratories (Pvt) Ltd. |
|
Atropine (Sulphate) Eye Oint 1 %W/W |
|
|
Atropine |
Lahore Chemical & Pharmaceutical Works (Pvt) Ltd |
|
Litropina |
Neo Medix |
|
Ophth-Atropine |
Ophth-Pharma (Pvt) Ltd. |
|
Atropine (Sulphate) Tabs 0.02 Mg |
|
|
Fymotil |
Fynk Pharmaceuticals |


 for multiple myeloma.webp)
.jpg)