- Prilocaine: Prilocaine is a local anesthetic of the amino amide type. It works by blocking the sodium channels necessary for the generation and conduction of nerve impulses, thereby producing a reversible loss of sensation in the area where it is applied or injected. Prilocaine is commonly used in various medical procedures, including minor surgeries, dental procedures, and dermatological procedures.
- Epinephrine: Epinephrine, also known as adrenaline, is a hormone and neurotransmitter that plays a crucial role in the body's fight-or-flight response. In combination with prilocaine, epinephrine serves several purposes:
- Vasoconstriction: Epinephrine causes constriction of blood vessels at the site of administration. This helps to reduce bleeding and prolong the duration of the local anesthetic effect by slowing the systemic absorption of prilocaine. By reducing blood flow to the area, it also decreases the risk of systemic toxicity from the anesthetic.
- Prolonged Anesthesia: The vasoconstrictive properties of epinephrine enhance the efficacy of prilocaine by keeping it localized and preventing its rapid systemic absorption. This results in prolonged anesthesia, allowing for longer-lasting pain relief.
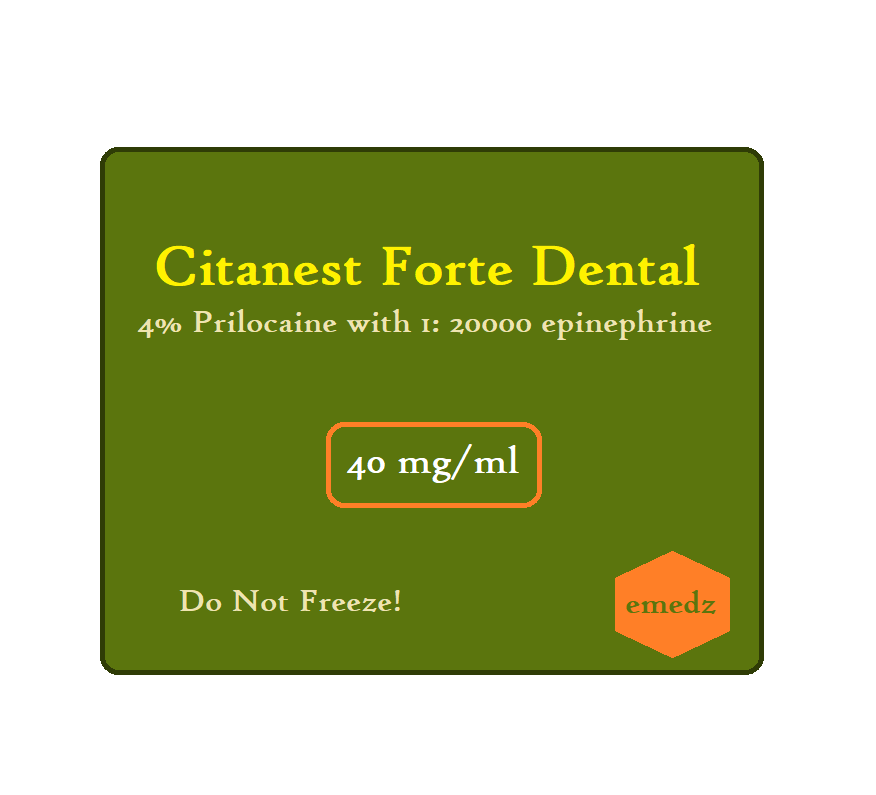
Prilocaine with epinephrine (Citanest Forte Dental) is a combination of a local anesthetic and a local vasoconstrictor drug that is used for nerve block in dental procedures such as dental extraction.
Prilocaine with epinephrine Uses:
- Dental anesthesia:
- It is used as a local anesthetic and for nerve block in dental procedures.
Prilocaine with epinephrine (Citanest Forte Dental) Dose in Adults
Note: Prilocaine with epinephrine is a combination used by doctors to make parts of the body numb for medical procedures. Prilocaine blocks nerves from sending pain signals, while epinephrine helps it work better and last longer by shrinking blood vessels and reducing bleeding. The right dose depends on the type of procedure, how much numbness is needed, how long it needs to last, and the patient's health. It's important for doctors to use the smallest effective dose and check for blood before giving the injection.
Prilocaine with epinephrine (Citanest Forte Dental) Dose in the Dental anesthesia:
- In dental anesthesia, the typical initial dose of prilocaine with epinephrine is 40 to 80 mg, which is equivalent to 1 to 2 milliliters (mL) of a 4% solution of prilocaine hydrochloride with epinephrine at a concentration of 1:200,000.
- The maximum dose within a 2-hour period depends on the patient's weight.
- For patients weighing less than 70 kilograms (kg), the maximum dose is 6 milligrams (mg) per kilogram of body weight, up to a maximum of 400 mg.
- For patients weighing 70 kilograms or more, the maximum dose is 400 mg or 5 to 6 cartridges.
- It's crucial for dentists to adhere to these dosage guidelines to ensure patient safety and effectiveness of the anesthesia.
Prilocaine with epinephrine (Citanest Forte Dental) Dose in Childrens
Prilocaine with epinephrine (Citanest Forte Dental) Dose in the Dental anesthesia:
- For children under 10 years old, doses greater than 40 mg (equivalent to 1 milliliter) of prilocaine hydrochloride as a 4% solution with epinephrine 1:200,000 are seldom necessary for dental procedures involving a single tooth, maxillary infiltration for 2 to 3 teeth, or an entire quadrant with a mandibular block.
- For children over 10 years old, the dosing is similar to adults and should follow adult guidelines.
Pregnancy Risk Factor B
- During pregnancy, prilocaine with epinephrine is considered to have a low risk, labeled as Pregnancy Risk Factor B.
- Studies in animals haven't shown any harmful effects on the baby during development.
- This means there haven't been any problems observed in animals when they were given this medication while pregnant.
Breastfeeding: Prilocaine and epinephrine
- The typical doses of prilocaine with epinephrine used in local anesthesia for nursing mothers have not been found to negatively impact the health of their breastfeeding infants.
- This means that there haven't been any observed adverse effects on the baby's health when nursing mothers receive this medication for local anesthesia.
Dose in Kidney disease:
- The manufacturer's labeling does not specify any adjustments to the dosage of prilocaine with epinephrine for individuals with renal impairment.
- However, it's advised to use this medication with caution in individuals with impaired kidney function because prilocaine is metabolized in the kidneys.
- This means that people with kidney problems may need closer monitoring or lower doses to avoid potential adverse effects.
Dose in Liver disease:
- The manufacturer's labeling does not include specific dosage adjustments for individuals with hepatic (liver) impairment when using prilocaine with epinephrine.
- However, caution should be exercised when administering this medication to patients with liver problems.
- Since prilocaine is metabolized in the liver, hepatic impairment may affect its metabolism and clearance from the body.
Side effects of Prilocaine with epinephrine (Citanest Forte Dental):
- Cardiovascular:
- Bradycardia
- Circulatory Shock
- Edema
- Hypotension
- Vasodepressor Syncope
- Central Nervous System:
- Apprehension
- Confusion
- Dizziness
- Drowsiness
- Euphoria
- Flushing Sensation
- Loss Of Consciousness
- Nervousness
- Numbness
- Seizure
- Sensation Of Cold
- Twitching
- Dermatologic:
- Skin Lesion
- Urticaria
- Gastrointestinal:
- Vomiting
- Hypersensitivity:
- Anaphylactoid Shock
- Hypersensitivity Reaction (Rare)
- Ophthalmic:
- Blurred Vision
- Diplopia
- Otic:
- Tinnitus
- Neuromuscular & Skeletal:
- Tremor
- Respiratory:
- Respiratory Depression
- Hypoxia
Contraindications to Prilocaine with epinephrine:
- Prilocaine with epinephrine should not be used in individuals who have a known hypersensitivity (allergic reaction) to local anesthetics of the amide type or to any component of the medication formulation.
- Additionally, it is contraindicated (should not be used) in individuals with congenital or idiopathic methemoglobinemia, a condition where there are high levels of methemoglobin in the blood, which can impair oxygen delivery to tissues.
- These contraindications are important to consider to prevent potentially serious allergic reactions or complications in susceptible individuals.
Warnings and precautions
CNS toxicity:
- After injection, monitor the patient closely for signs of central nervous system (CNS) toxicity, such as restlessness, anxiety, tinnitus (ringing in the ears), dizziness, blurred vision, tremors, depression, or drowsiness.
- If these signs occur, treatment is primarily symptomatic and supportive.
Methemoglobinemia:
- This condition, characterized by abnormal levels of methemoglobin in the blood, can occur after using local anesthetics.
- Prompt treatment is necessary if clinically significant methemoglobinemia is observed, including discontinuation of the anesthetic.
- Certain individuals, such as those with glucose-6-phosphate dehydrogenase deficiency or infants under 6 months old, are more susceptible and should be closely monitored for symptoms like cyanosis (bluish discoloration of the skin), headache, rapid pulse, shortness of breath, lightheadedness, or fatigue.
- Avoid use in patients with congenital or idiopathic methemoglobinemia.
Respiratory Arrest and Seizures:
- Rarely, local anesthetics have been associated with sudden respiratory arrest or seizures due to systemic toxicity, especially following unintentional intravascular injection.
- Careful administration is crucial.
Cardiovascular disease
- Use caution, particularly in patients with significant cardiovascular disease, because of the epinephrine component.
- Minimal amounts should be used in such patients.
Familial malignant hyperthermia
- Prilocaine may potentially trigger malignant hyperthermia, a rare but serious condition.
- Follow standard protocols for identification and treatment.
Hepatic impairment
- Patients with hepatic impairment should use prilocaine with caution, as amide-type anesthetics are metabolized in the liver.
Hyperthyroidism:
- Avoid use in patients with uncontrolled hyperthyroidism.
Vascular disease
- Exercise caution when using local anesthetic solutions containing a vasoconstrictor, particularly in patients with peripheral vascular disease or hypertensive vascular disease, as they may have an exaggerated response, leading to ischemic injury or necrosis.
Prilocaine with epinephrine (dental): Drug Interaction
|
Alpha1-Blockers |
May diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Similarly, Alpha-/Beta-Agonists may antagonize Alpha1-Blocker vasodilation. |
|
Antidiabetic Agents |
Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. |
|
AtoMOXetine |
May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. |
|
Benperidol |
May diminish the therapeutic effect of EPINEPHrine (Systemic). |
|
Beta-Blockers (Beta1 Selective) |
May diminish the therapeutic effect of EPINEPHrine (Systemic). |
|
Beta-Blockers (Nonselective) |
May enhance the hypertensive effect of EPINEPHrine (Systemic). Exceptions: Arotinolol; Carvedilol; Labetalol. |
|
Beta-Blockers (with Alpha-Blocking Properties) |
May diminish the therapeutic effect of EPINEPHrine (Systemic). |
|
Cannabinoid-Containing Products |
May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. |
|
Chloroprocaine |
May enhance the hypertensive effect of Alpha-/Beta-Agonists. |
|
CloZAPine |
May diminish the therapeutic effect of Alpha-/Beta-Agonists. |
|
COMT Inhibitors |
May decrease the metabolism of COMT Substrates. |
|
Dapsone (Topical) |
May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. |
|
Doxofylline |
Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. |
|
Guanethidine |
May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. |
|
Local Anesthetics |
Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. |
|
Methemoglobinemia Associated Agents |
May enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. |
|
Monoamine Oxidase Inhibitors |
May enhance the hypertensive effect of EPINEPHrine (Systemic). |
|
Neuromuscular-Blocking Agents |
Local Anesthetics may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents. |
|
Nitric Oxide |
May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when nitric oxide is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine. |
|
Sodium Nitrite |
Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. |
|
Solriamfetol |
Sympathomimetics may enhance the hypertensive effect of Solriamfetol. |
|
Spironolactone |
May diminish the vasoconstricting effect of Alpha-/Beta-Agonists. |
|
Sympathomimetics |
May enhance the adverse/toxic effect of other Sympathomimetics. |
|
Technetium Tc 99m Tilmanocept |
Local Anesthetics may diminish the diagnostic effect of Technetium Tc 99m Tilmanocept. Management: Avoid mixing and simultaneously co-injecting technetium Tc 99m tilmanocept with local anesthetics. This interaction does not appear to apply to other uses of these agents in combination. |
|
Tedizolid |
May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. |
|
Benzylpenicilloyl Polylysine |
Alpha-/Beta-Agonists may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Consider use of a histamine skin test as a positive control to assess a patient's ability to mount a wheal and flare response. |
|
Cocaine (Topical) |
May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. |
|
Hyaluronidase |
May enhance the vasoconstricting effect of Alpha-/Beta-Agonists. Management: Avoid the use of hyaluronidase to enhance dispersion or absorption of alpha-/beta-agonists. Use of hyaluronidase for other purposes in patients receiving alpha-/beta-agonists may be considered as clinically indicated. |
|
Inhalational Anesthetics |
May enhance the arrhythmogenic effect of EPINEPHrine (Systemic). Management: Administer epinephrine with added caution in patients receiving, or who have recently received, inhalational anesthetics. Use lower than normal doses of epinephrine and monitor for the development of cardiac arrhythmias. |
|
Linezolid |
May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. |
|
Promethazine |
May diminish the vasoconstricting effect of EPINEPHrine (Systemic). Management: When vasoconstrictive effects are desired in patients receiving promethazine, consider alternatives to epinephrine. Consider use of norepinephrine or phenylephrine, and avoid epinephrine, when treating hypotension associated with promethazine overdose. |
|
Serotonin/Norepinephrine Reuptake Inhibitors |
May enhance the tachycardic effect of Alpha-/Beta-Agonists. Serotonin/Norepinephrine Reuptake Inhibitors may enhance the vasopressor effect of Alpha-/Beta-Agonists. |
|
Tricyclic Antidepressants |
May enhance the vasopressor effect of Alpha-/Beta-Agonists (DirectActing). Management: Avoid, if possible, the use of direct-acting alpha-/beta-agonists in patients receiving tricyclic antidepressants. If combined, monitor for evidence of increased pressor effects and consider reductions in initial dosages of the alpha-/beta-agonist. |
|
Blonanserin |
May diminish the therapeutic effect of EPINEPHrine (Systemic). |
|
Bromperidol |
May diminish the therapeutic effect of EPINEPHrine (Systemic). |
|
Bupivacaine (Liposomal) |
Local Anesthetics may enhance the adverse/toxic effect of Bupivacaine (Liposomal). Management: Liposomal bupivacaine should not be administered with local anesthetics. Liposomal bupivacaine may be administered 20 minutes or more after the administration of lidocaine, but the optimal duration of dose separation for other local anesthetics is unknown |
|
Ergot Derivatives |
May enhance the hypertensive effect of Alpha-/Beta-Agonists. Ergot Derivatives may enhance the vasoconstricting effect of Alpha-/Beta-Agonists. Exceptions: Ergoloid Mesylates; Nicergoline. |
|
Lurasidone |
EPINEPHrine (Systemic) may enhance the hypotensive effect of Lurasidone. |
Monitoring parameters:
Monitoring Vital Signs and Consciousness for CNS Toxicity
- Cardiovascular and Respiratory Vital Signs:
- Regularly monitor the patient's heart rate, blood pressure, and respiratory rate before and after each injection of prilocaine with epinephrine.
- Changes in these vital signs may indicate potential cardiovascular or respiratory complications.
- State of Consciousness After Each Injection:
- Assess the patient's state of consciousness following each injection of the local anesthetic.
- Watch for signs such as restlessness, anxiety, tinnitus, dizziness, blurred vision, tremors, depression, or drowsiness, as these may be early indicators of central nervous system (CNS) toxicity.
- CNS Toxicity:
- Be vigilant for symptoms of CNS toxicity, including those mentioned above.
- If any signs or symptoms occur, it's essential to intervene promptly and provide symptomatic and supportive treatment as necessary to ensure the patient's safety.
How to administer Prilocaine with epinephrine (Citanest Forte Dental)?
It is administered using a 25-gauge needle around the nerve (locally infiltrated). before injecting the drug, pull the plunger of the syringe. If blood is drawn while pulling the plunger, the injection should not be injected.
Mechanism of action of Prilocaine with epinephrine (Citanest Forte Dental):
- Local anesthetics like prilocaine work by selectively binding to sodium channels on the intracellular surface, blocking the influx of sodium ions into the nerve axon.
- This blockade prevents depolarization, which is necessary for the propagation of action potentials and subsequent nerve function.
- Importantly, this blockage is reversible, and once the drug diffuses away from the axon, sodium channel function is restored, and nerve propagation resumes.
- Epinephrine, added to prilocaine, extends its anesthetic effect by causing vasoconstriction around the nerve axons.
- This vasoconstriction, mediated by alpha-adrenergic receptors, limits the diffusion of prilocaine away from the nerves, leading to a longer duration of action by keeping the drug concentrated in the axon.
The beginning of action:
- For infiltration injections, where the anesthetic is injected directly into the tissue, the onset of action is typically less than 2 minutes.
- For inferior alveolar nerve blocks, which target a specific nerve in the jaw, the onset of action is usually less than 3 minutes.
Duration:
- For infiltration injections, the anesthetic effect lasts approximately 2.25 hours.
- For inferior alveolar nerve blocks, the duration of action is around 3 hours.
International Brand Names of Prilocaine with epinephrine:
- Citanest Forte Dental
- Citanest Adrenalin
- Citanest Forte
Prilocaine with epinephrine Brand Names in Pakistan:
No Brands Available in Pakistan.