Coronavirus treatment Guidelines have been proposed by the Massachusetts General Hospital and the recommendations are evolving. This review is a summary taken from multiple sources and experts in the field. I do not have any association with any pharmaceutical companies and have no conflicts of interest (financial or otherwise). This review is solely intended for all the patients with COVID-19 Coronavirus infection who are apart from their families and friends. May God protect us all.
Note: Antimalarial medications (such as hydroxychloroquine and chloroquine) are thought to limit the illness to the upper respiratory tract and lower the likelihood of pneumonia linked to COVID-19. These medications could be used to stop Coronavirus infections.
Treatment not recommended in patients with Coronavirus infection:
- Systemic corticosteroids should be avoided in all patients except in those with compelling indications such as shock or in transplant patients.
- Inhaled corticosteroids should also be discontinued if possible as they may reduce local immunity and promote viral replication.
- Although the virus binds the ACE2 receptors avidly, ACE inhibitors and ARBs are not recommended and should be avoided especially in patients with volume depletion, hypotension, acute kidney injury, and hyperkalemia.
- Ribavirin is not indicated for COVID-19 treatment.
- NSAIDs, especially Ibuprofen, should be avoided as clinical deterioration followed their use in some patients.
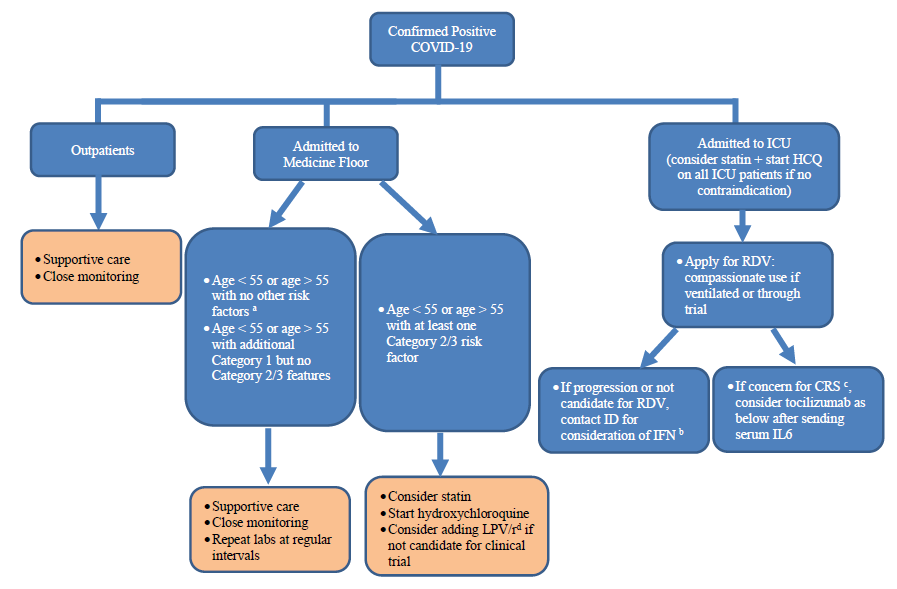
Coronavirus Treatment Guidelines for all hospitalized patients:
-
Patients with mild disease (without risk factors and SpO2 of 90% or more):
- These patients may require only supportive care.
- Supportive care includes:
- Supplemental Oxygen is required in patients with shock, respiratory distress, and hypoxemia. Oxygen should be administered at a rate of 5 l/min and adjusted to keep the SpO2 greater than 90%.
- Fluids should be given cautiously unless the patient has gastrointestinal symptoms, reduced intake, or in shock. Aggressive fluid resuscitation may worsen the gas exchange.
- Antipyretics should be given to patients for pain and fever. However, as mentioned above, NSAIDs and especially ibuprofen should be avoided.
- Empirical antibiotics should be given to patients with sepsis or suspected bacterial infection. Neuraminidase inhibitors (Oseltamivir, Zanamivir) may be given unless influenza has been ruled out.
-
Patients with mild disease and SpO2 of more than 90% but with risk factors of severe COVID-19 disease:
- Supportive care as in those with mild disease and without risk factors should be provided.
- Frequent monitoring of the disease and risk stratification should be continued.
- Patients may be enrolled in clinical trials to receive remdesivir.
-
Intended for those with severe or moderate illness. These include those who require support from an intensive care unit and those who have progressive illnesses.
- Administer remdesivir in the following doses:
- Following an intravenous loading dose of 200 mg, 100 mg was administered once every day for a total of ten days.
Hospitalized patients with SARS-CoV-2 verified by PCR who are also receiving mechanical ventilation are eligible for "compassionate usage."Patients who fall under the category of "compassionate use of remdesivir" are not eligible:
- Patients with multi-organ failure,
- those who require vasopressors for hypotension,
- patients with ALT greater than 5 times the upper limits of normal,
- those with a CrCl of less than 30 ml/minute, or on hemodialysis/ CVVH.
- Administer remdesivir in the following doses:
Patients can apply for compassionate use here: https://rdvcu.gilead.com/
-
Patients with severe disease, those with progressive disease despite remdesivir treatment, patients in the ICU, and in areas where remdesivir treatment is not available:
- On day one, take 400 mg twice a day of hydroxychloroquine; on days two through five, take 200 mg twice a day.
- Recent research suggests combining azithromycin at a dose of 500 mg twice daily for five days with hydroxychloroquine at a dose of 400 mg twice daily on day one and 200 mg twice daily for the next four days.
-
- Since both drugs increase the QT interval, this combination should be used with extreme caution. A baseline ECG should be done and repeated daily. Patients with a QT interval of 500 msec or more should not be advised combined azithromycin and hydroxychloroquine.
-
OR
- Chloroquine phosphate (Resochin) 500 milligrams two times per day for five days
-
OR
- Lopinavir or Ritonavir (Kaletra) 400/100 milligrams two times daily for ten days (This regimen should be avoided if the patient is a potential candidate for remdesivir drug trial.
- Monitor for drug-drug interactions especially with concomitant calcineurin inhibitors and liver function tests periodically.
- Treatment should be discontinued when the patient is discharged (regardless of the duration of the treatment)
-
OR
- Darunavir/cobicistat (DRV/c or Prezcobix) 800/150 mg daily may be taken into consideration if Kaletra is not readily available.
-
Refractory patients in the ICU:
- Administer Interferon-beta B1 (Betaseron) in combination with hydroxychloroquine or Kaletra (Lopinavir/ ritonavir).
-
COVID-19 patients with Cytokine Storm:
- Send IL-6 (Interleukin 6) levels and initiate Tocilizumab (Actemra) treatment.
- Cytokine storm is the hyper-responsiveness of the immune system against the COVID-19 virus resulting in acute lung injury, ARDS, refractory hypotension, and multiorgan failure.