Gadobutrol (Gadavist) is a gadolinium-based MRI contrast agent that is used in the diagnosis of CNS imaging, cardiac imaging, renal angiography, and detection of breast malignancy.
Gadobutrol Uses:
-
US labeling:
- Breast malignancy imaging: Contrast medium for use with MRI to assess the presence and extent of malignant breast disease.
- CNS imaging: MRI in adults, adolescents, and pediatric patients (including term neonates) to detect and visualize areas with disrupted blood-brain barrier and/or abnormal vascularity of the CNS.
- Supra-aortic or renal artery angiography: Magnetic resonance angiography (MRA) in adult and pediatric patients (including term neonates) to evaluate known or suspected supra aortic or renal artery disease.
-
Canadian labeling:
- Breast malignancy imaging: Contrast medium for use with MRI to assess the presence and extent of malignant breast disease.
- CNS imaging: Contrast medium for MRI of CNS lesions (spine, brain, and associated tissues) and for perfusion studies to diagnose stroke, or to detect focal cerebral ischemia or tumor perfusion.
- Contrast-enhanced magnetic resonance angiography: Contrast medium for contrast-enhanced magnetic resonance angiography (CE-MRA).
- Renal imaging: Contrast medium for MRI of the kidney.
Gadobutrol (Gadavist) Dose in Adults
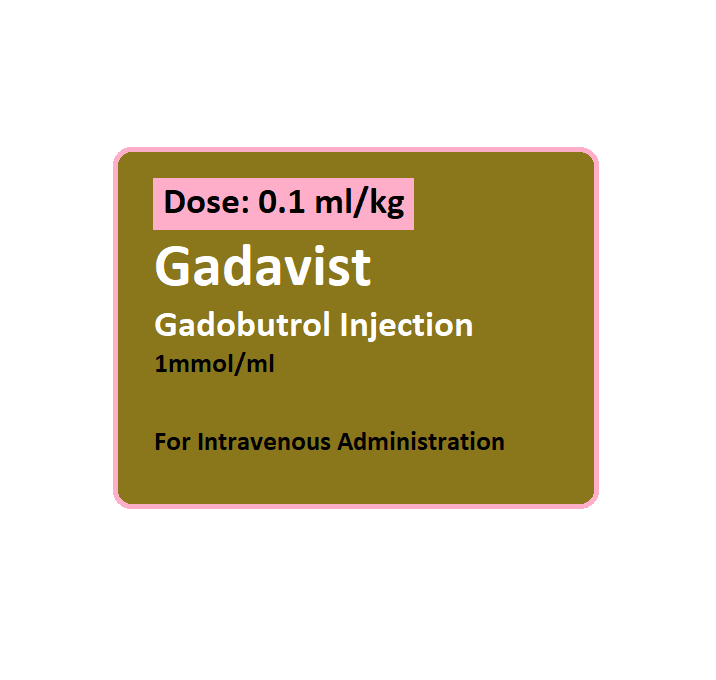
Gadobutrol (Gadavist) Dose in Diagnostic imaging: IV:
-
US labeling:
-
Breast malignancy imaging, CNS imaging, and supra-aortic or renal artery angiography:
- 0.1 mmol per kg (0.1 mL per kg);
- May begin imaging immediately after administration
-
-
Canadian labeling:
-
Breast malignancy imaging:
- Usual dose: 0.1 mmol per kg (0.1 mL per kg);
- The maximum dose: 0.3 mmol per kg (0.3 mL per kg)
-
CNS imaging:
- General imaging: 0.1 mmol per kg (0.1 mL per kg); if needed, a second dose of 0.1 to 0.2 mmol per kg (0.1 to 0.2 mL per kg) may be repeated once within 30 minutes of the first dose
- Exclusion of metastatic or recurrent tumors: 0.3 mmol per kg (0.3 mL per kg)
- Perfusion studies: 0.1 to 0.3 mmol per kg (0.1 to 0.3 mL per kg)
-
CE-MRA:
- Imaging of a single field of view (FOV):
- Patient weight <75 kg: 7.5 mL
- Patient weight ≥75 kg: 10 mL
- Imaging >1 FOV:
- Patient weight <75 kg: 15 mL
- Patient weight ≥75 kg: 20 mL
- Imaging of a single field of view (FOV):
-
Renal imaging:
- Usual dose: 0.1 mmol per kg (0.1 mL per kg);
- The maximum: 0.3 mmol per kg (0.3 mL per kg)
-
Gadobutrol (Gadavist) Dose in Childrens
Gadobutrol (Gadavist) Dose in Diagnostic imaging: IV:
-
US labeling:
-
CNS imaging, supra-aortic, or renal artery angiography:
- Neonates, Children, and Adolescents: Refer to adult dosing
-
-
Canadian labeling:
-
CNS imaging/CE-MRA or renal imaging:
- Newborns, Infants, Children, and Adolescents:
- 0.1 mmol/kg (0.1 mL/kg); do not exceed recommended dose.
- Sequential or repeat dosing has not been studied; allow for a weak or more than a weak before considering repeat administration.
- Newborns, Infants, Children, and Adolescents:
-
Pregnancy Category: C
- Contrast agents containing gadolinium may cross the placenta.
- If it is expected to significantly improve diagnostic performance, and to improve fetal and maternal outcomes, a gadolinium-based contrast agents with MRI might be considered for pregnancy.
- Contrast agents containing gadolinium-based compounds in pregnancy are controversial and should be avoided.
- Low-risk agents should not be administered at lower doses. Considerations for Breast-Feeding
- Additionally, it is important to only consider using a contrast agent if the information required from an MRI study can't be obtained without using one. This cannot be delayed until after delivery.
Gadobutrol use during breastfeeding:
- Breast milk may contain gadolinium-based, contrast agents.
- Theoretically speaking, milk's taste could be affected if it contains contrast media.
- Women who choose to temporarily stop breastfeeding can express breast milk and then discard it after 12-24 hours.
- Breastfeeding may continue after discontinuation due to the low expected excretion of breast milk and low absorption by infants' GI tract.
- They can store and pump milk before the procedure, then bottle-feed the milk stored during that time.
- According to the manufacturer breastfeeding during therapy is a decision that should be made after considering the risks to infants and the benefits to mothers.
Gadobutrol (Gadavist) Dose in Kidney Disease:
Dose adjustment is not necessary; however, use with caution. The risk for NSF development increases as renal function decreases.
-
Hemodialysis:
- If administered to patients already receiving hemodialysis, consider prompt hemodialysis following exposure.
- Data has shown hemodialysis enhances gadolinium elimination with average gadolinium excretory rates of 78 percent, 96 percent, and 99 percent in the first, second, and third hemodialysis sessions, respectively.
-
Peritoneal dialysis:
- Likely to be less efficient at clearing gadolinium.
Dose in Liver disease:
The manufacturer’s labeling doesn't provide any dosage adjustments; however, based on exclusive renal excretion of gadobutrol, dose adjustment in hepatic impairment is likely unnecessary.
Side Effects of Gadobutrol (Gadavist):
-
Central nervous system:
- Headache
-
Gastrointestinal:
- Nausea
Contraindications to Gadobutrol (Gadavist):
Hypersensitivity to gadobutrol and any component of the formulation.
Warnings and precautions
-
Extravasation:
- Monitor infusion site.
- Could be a vesicant (higher volumes and/or osmolar contrast agents are associated with a greater risk).
- Before and during administration, ensure proper placement of the needles or catheters.
- Avoid extravasation. Local tissue irritation could occur.
-
Gadolinium retention:
- Minimize repetitive GBCA imaging studies.
- Gadolinium can be retained in the brain, bones, skin, liver, and other organs for many months to years. The bone has the highest concentration and longest retention.
- Gadolinium retention in the brain and in patients with normal renal function has not been shown to have any adverse effects.
- Linear GBCAs, such as gadodiamide, gadoversetamide, gadoxetate dimeglumine and gadobenate dimeglumine, have a higher retention rate than macrocyclic ones (gadoterate, gadobutrol and gadoteridol).
- Patients with impaired renal function have had to deal with the clinical and pathologic consequences of gadolinium storage in their skin and other organs.
- Rarely, however, have they experienced skin problems that were not related to renal impairment.
- Patients with normal renal function may be more at risk of gadolinium retention.
- These include patients who require multiple lifetime doses, pregnant or pediatric patients, as well as patients with inflammatory conditions.
-
Hypersensitivity
- Reactions usually occur within 30 minutes after administration. However, delayed reactions can occur (up to several weeks following administration).
- Appropriate equipment (eg, ventilator) and emergency medications (eg, epinephrine) should be available during use.
- Anaphylactic reactions and other hypersensitivity reactions (some deadly) have been reported (with mild to severe cardiovascular, respiratory or dermatologic involvement).
- Patients with a history or bronchial asthma and allergic reactions should be cautious. They may be at greater risk of developing hypersensitivity reactions.
-
Nephrogenic systemic Fibrosis (NSF: [US Boxed Warning]
- Gadolinium-based contrast agents (GBCAs) increase the risk of NSF in patients suffering from renal impairment.
- Avoid using GBCA-enhanced imagery unless it is absolutely necessary for diagnostic purposes.
- Patients with severe, acute kidney disease or acute kidney injury are at greatest risk (GFR 30mL/minute/1.73m2).
- Patients with moderate to severe chronic kidney disease have a lower risk of NSF (GFR 30 to 60 mL/minute per 1.73m2) and patients with milder chronic renal disease have a low GFR (GFR 60 mL/minute per 1.73m2).
- Consider prompt initiation for patients on hemodialysis.
- NSF should be reported to the manufacturer or Food and Drug Administration (FDA).
- Before administering medication, all patients should be tested for kidney dysfunction.
- Patients at high risk for NSF should not exceed the recommended dose and allow enough time (i.e. several half-lives), for elimination before re-administration. Avoidance of readministration is preferred.
- Consider prompt hemodialysis for patients on hemodialysis.
-
Renal impairment
- Acute kidney injury has been reported in patients with chronically impaired renal function.
- Before using, evaluate the renal function of patients with kidney impairment; consider following-up monitoring.
- Patients with impaired renal function should be cautious.
- Patients with acute renal impairment have experienced a dose-dependent worsening or severe renal dysfunction after the administration of gadolinium agents. This usually occurs within 48 hours.
-
Seizure disorder:
- Patients with seizure disorders should be cautious as it can lower the seizure threshold.
- It is important to have injectable anticonvulsant drugs readily available.
Monitoring parameters:
- Renal function;
- signs of hypersensitivity (during and for several hours after the procedure);
- short- and long-term monitoring of signs and symptoms of Nephrogenic systemic fibrosis (NSF/NFD) such as itching, swelling, hardening and/or tightening of skin burning, joint stiffness, deep hip or rib bone pain, muscle weakness, limited range of motion, and/or yellowed/raised spots on whites of eyes.
- monitor infusion site for signs/symptoms of extravasation.
How to administer Gadobutrol?
IV:
- Do not administer other medications in the same IV line simultaneously.
Breast malignancy imaging:
- Administer as an IV bolus by power injector, followed by NS flush. Post-contrast MRI can commence immediately following contrast administration.
CNS imaging:
- Administer as an IV injection, manually or by power injector, at a rate of ~2 mL per second, followed by an NS flush. Post-contrast MRI can commence immediately following contrast administration.
Supra-aortic or renal artery angiography:
- Image acquisition should coincide with peak arterial concentration, which varies among patients.
- Adult: Administer by power injector, at a rate of ~1.5 mL per second, followed by a 30 mL NS flush at the same rate.
Canadian labeling:
- For perfusion studies, an automatic injector is recommended at an infusion rate of 3 to 5 mL per second.
- It may be a vesicant. Ensure proper needle or catheter placement prior to and during infusion. Avoid extravasation.
Extravasation management:
- If extravasation occurs, stop infusion immediately and disconnect; remove needle/cannula, and elevate extremity.
- Aspiration of extravasated contrast media is not recommended. Information conflicts regarding the use of hyaluronidase.
- The American College of Radiology (ACR) Manual on Contrast Media does not recommend hyaluronidase in the management of contrast media extravasation, however, other sources suggest its utility in extravasation management.
- If using hyaluronidase: Intradermal or SubQ:
- Inject a total of 1 to 1.7 mL (15 units per mL) as five separate 0.2 to 0.3 mL injections (using a 25-gauge needle) into the area of extravasation at the leading edge in a clockwise manner or injection of a total of 5 mL (150 units per mL) as five separate 1 mL injections around the extravasation site has been also used successfully.
Mechanism of action of Gadobutrol (Gadavist):
- Gadobutrol is a gadolinium-containing, nonionic paramagnetic agent.
- The local magnetic field is created when tissues are exposed to an external magnetic force.
- The local magnetism causes water protons to lose their magnetic field, which results in a change of proton density and spin characteristics.
- This can be detected using an imaging device.
Distribution:
- Rapid into extracellular space
Metabolism:
- Not metabolized
Half-life elimination:
- Normal renal function: ~1.5 to 2 hours;
- severe renal dysfunction (CrCl <30 mL/minute): 17.6 hours (mean)
Excretion:
- Urine (>90 percent as unchanged drug);
- feces (negligible)
International Brand Names of Gadobutrol:
- Gadavist
Gadobutrol Brand Names in Pakistan:
There is no brand available in Pakistan.