The discovery of insulin has revolutionized the treatment of Diabetes. Currently, different types of Insulin are available in the market. Various formulations have been tried including insulin via inhalation but apart from the injectable formulations, others have failed to prevail in the markets because of various reasons.
All types of insulin require to be administered via injections except for the inhaled one (Afrezza). The most common method of administration is subcutaneous injections.
However, hospitalized patients may also require intravenous or intramuscular injections. Insulin can be injected via insulin syringes, prefilled insulin pens, insulin pens with cartridges that need to be refilled and insulin pumps depending on the types of insulin.
Which patients require Insulin?
Insulin is essential for all patients with Type 1 Diabetes Mellitus and the following groups of patients:
- Type 2 Diabetes Mellitus patients with uncontrolled Diabetes despite maximum medications
- Patients with Gestational Diabetes Mellitus
- Type 2 Diabetes Mellitus with
- Advanced Kidney Disease ( creatinine clearance of less than 30ml/min)
- Advanced Heart Disease and heart failure (Ejection Fraction of less than 25%)
- Decompensated Liver disease manifested by ascites, jaundice, encephalopathy and variceal bleeding.
- Patients with type 2 Diabetes Mellitus and a concomitant serious illness like severe pneumonia, acute kidney failure, severe infections, Myocardial infarction, acute exacerbation of chronic bronchitis, respiratory failure, and other serious diseases that require hospitalization.
- Perioperative control of blood sugars in Diabetic Patients, and
- Emaciated patients and patients with gastrointestinal diseases that impair the absorption of oral antidiabetic medications.
What are the side effects of Insulin?
Lipohypertrophy at insulin injection sites[/caption] Insulin is produced via recombinant genetic engineering technology, where the human genes are transcribed into bacterial DNA and the proinsulin molecule is produced. This proinsulin molecule is then cleaved into the final form of usable insulin. Important Side effects of Insulin include:
-
Pain at the injection site:
- Since Insulin requires to be injected into the body, it may be painful.
- The currently used ultrafine insulin needles are virtually painless.
-
Allergy to Insulin:
- Since insulin is a genetically engineered protein, patients may be allergic to it.
- Switching to a different type of insulin may be helpful in some patients.
-
Hypoglycemia:
- Since patients use insulin to lower their blood sugars, administering large doses of insulin may result in lowering blood sugars.
- Patients may not palpitations, sweating, tremors, feeling of being hungry, or drowsiness, and severe cases may become unconscious completely
-
Weight gain:
- Insulin is an anabolic hormone that causes a noticeable increase in body weight.
- Although this effect of insulin may be beneficial in thin, lean patients, it is a concerning side effect in the majority of obese diabetes patients.
-
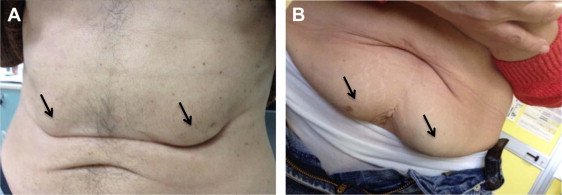
Lipohypertrophy:
- Lipohypertrophy is the accumulation of fats at the site of insulin injection.
- The patients may note lumps on the abdominal wall.
- To avoid this side effect, the patient is suggested to rotate the site of injection.
What are the different types of Insulin?
Insulins are categorized based on their onset and duration of actions.
-
Ultra-rapid-acting insulins:
- Ultra-rapid-acting insulins have an onset of action of 12 to 15 minutes, a peak effect of 30 minutes to one hour, and a total duration of action of up to 4 hours. Inhaled insulin Afezza is the most rapid-acting. Others in this category include FiAsp Insulin or Faster Aspart and Insulin Lyumjev (Lispro-aabc)
-
Rapid-acting Insulin:
- This group of insulin has a rapid onset of action (within 25 minutes), which peaks in about thirty minutes to one hour and remains functional for about four hours.
- The following Insulins are rapid-acting insulins:
- Insulin Aspart,
- Insulin Glulisine, and
- Insulin Lispro
-
Short-Acting Insulin:
- Human Regular Insulin is the only short-acting insulin.
- It has an onset of action between 30 minutes to one hour and peaks in between 2 to 3 hours.
- It remains active for 4 to 6 hours.
-
Intermediate-acting insulin:
- NPH insulin has an onset of action between one and four hours, a peak activity between six and ten hours, and a total duration of action between 10 to 16 hours.
- It is usually given in combination with rapid-acting or short-acting insulins.
-
Long-acting Insulin:
- Long-acting insulins start working right away., like the NPH insulin, between 1 to 4 hours.
- These Insulins have no Peak (or minimal peak) and are functional for 18 to 24 hours.
- The two types of long-acting insulins are:
- Insulin Glargine and
- Insulin Detemir
-
Ultra-long-acting Insulin:
- The only ultra-long-acting insulin is insulin Degludec.
- Similar to long-acting insulins, it begins to work between one and four hours later, is peakless, and lasts for 96 hours.
-
Insulin combinations:
- Various Insulin combinations are available nowadays.
- In these combinations, intermediate-acting, long-acting, or ultra-long-acting insulins are typically paired with rapid-acting, short-acting, or both types of insulin.
- The usual combinations include either 25%, 30% or 50% of the rapid and short-acting insulins and 50%, 70% or 75% intermediate or long-acting insulins.
- The major benefit of these combinations is to reduce the frequency of insulin injections.
How frequently should insulin be injected?
The frequency of insulin injections can vary.
- Long and ultra-long-acting insulins are also called as Basal Insulins.
- These can be administered as a once-daily injection, preferably along with oral antidiabetic medicines.
- Since basal insulins are peakless insulins, they seldom cause hypoglycemia.
- Furthermore, these insulins primarily control the pre-meals or fasting blood sugars, but have little effect on post-meal blood sugars.
- In addition, these insulins can be administered without regard to meals.
-
Intermediate-acting insulins can be given as once or preferably twice daily, usually in combination with short or rapid-acting insulins or oral anti-diabetic medicines.- These Insulins have peak hours and may, therefore, cause hypoglycemia more frequently when compared to the long and ultra-long-acting insulins.
- Intermediate-acting insulins are also used primarily to cover pre-meals blood sugars.
-
Short-acting insulins are given twice or thrice daily injections before each meal.- The meal should be ready prior to the injection.
- After injecting the insulin, the patient should wait for about 20 to 30 minutes and then take the meals.
- Short-acting insulin is also used to manage emergencies like diabetic ketoacidosis, pre and post-operative management of diabetes.
- It can be given as an intramuscular or intravenous injection or as a continuous intravenous infusion.
-
Rapid-acting insulins are used in patients who are at risk of hypoglycemia like those with end-stage kidney, liver and heart diseases.- These insulins are also best for those who can not wait for 20-30 minutes before a meal like during busy office hours.
- Each meal should be preceded by the administration of rapid-acting insulin, which is typically combined with intermediate-acting, long-acting, or ultra-long-acting insulin.
Which type of insulin is required for me?
Which patients need which type of insulin? Each physician has his own way of treating the patient. Whichever insulin is prescribed, the primary goal for all the patients is the same - to control blood sugars and avoid hypoglycemia. Below is a brief overview of the type of insulin required for your patient to achieve good compliance and avoid adverse effects.
- Patients who have uncontrolled pre-meals or fasting blood sugars may best be started on once-daily long-acting or ultra-long-acting insulins.
- Patients with uncontrolled post-meals blood sugars require short or rapid-acting insulins to cover that meal.
- Patients with end-stage kidney, liver or heart diseases or those at risk of hypoglycemia may be advised rapid-acting insulins.
- Patients who are non-compliant or have fear of injections may be started on once-daily long or ultra-long-acting insulins.
- Patients who are scheduled for surgery or have diabetes-related emergencies like diabetic ketoacidosis and hyperosmolar hyperglycemia may be started on an intravenous infusion of short-acting insulins.
What are the different (types of insulin) brands available?
The following are the few well-known brands of insulin currently available:
Insulin (the type of insulin) |
Brands |
|
| Rapid-acting | Aspart | Novorapid |
| Lispro | Humalog | |
| Glulisine | Apidra | |
| Short-acting | Regular insulin | Actrapid Humulin R Insuman Rapid Insuget R |
| Intermediate-acting | NPH insulin | Humulin N Insuman Basal Insuget N |
| Long-acting | Glargine (U-100) Glargine (U-300) | Lantus, Basagine Toujeo |
| Detemir | Levemir | |
| Ultra-long-acting | Degludec | Tresiba |
| Pre-mixed 70/30 | 70% NPH 30% Regular 70% Aspart-protamine 30% Aspart 70% Degludec 30% Aspart | Humulin 70/30, Mixtard 70/30, Insuget 70/30 Novomix-30 Ryzodeg |
| Pre-mixed 75/25 | 75% Lispro-protamine 25% Lispro | Humalog Mix 25 |
| Premixed 50/50 | 50% Lispro-protamine 50% Lispro | Humalog Mix 50 |
In conclusion:
Prescribing insulin can be a little tricky, especially, if the prescriber has little knowledge of the onset, duration, and formulation of insulin.