Levamlodipine is a medication used to treat high blood pressure (hypertension) and chest pain (angina). It belongs to a class of drugs known as calcium channel blockers. Levamlodipine works by relaxing and widening blood vessels, which helps to improve blood flow and lower blood pressure. It is similar to amlodipine, but levamlodipine specifically refers to the S-enantiomer of amlodipine. Enantiomers are molecules that are mirror images of each other, and sometimes one enantiomer may be more effective or have fewer side effects than the other.
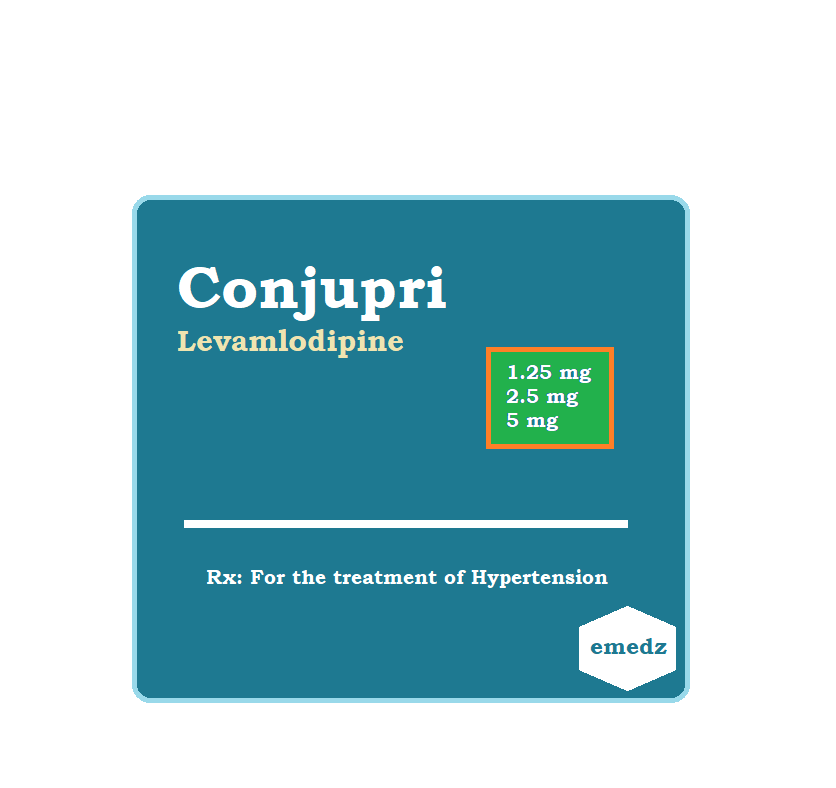
Levamlodipine (Conjupri) is the active isomer of amlodipine. It is used orally for the treatment of patients with hypertension.
Levamlodipine Uses:
- Hypertension:
- Adults and kids aged six and older who have hypertension are administered it to treat it.
Levamlodipine Dose in Adults:
Levamlodipine dose in Hypertension:
Note:
- Levamlodipine is a medication for high blood pressure.
- If your blood pressure is significantly higher than the target level, your doctor may suggest combining it with another medication like an angiotensin-converting enzyme inhibitor, angiotensin II receptor blocker, or a thiazide diuretic at first.
- But if your blood pressure is only a bit higher than the target, you might start with just levamlodipine.
- You take levamlodipine by mouth, usually starting with 1.25 to 2.5 milligrams once a day.
- Your doctor might adjust this dose every one to two weeks depending on how you respond and your needs.
- The most you'd take in a day is 5 milligrams.
- Taking more than that won't work better and could cause more side effects.
Levamlodipine dose in children:
Levamlodipine dose in Hypertension:
- For young children and teenagers aged 6 to 17:
- The typical dose of levamlodipine is 1.25 to 2.5 milligrams taken orally once a day.
Levamlodipine Pregnancy Risk Category: N
- Levamlodipine and dextro-amlodipine are like the two parts that make up amlodipine.
- Amlodipine doesn't have a barrier in the placenta.
- If you want to know more, you can check out the information in the amlodipine guide.
Use during breastfeeding:
- Amlodipine is found in breast milk and can be seen as a mix of levamlodipine, which is the active part, and dextro-amlodipine.
- If you need more details, you can look up the amlodipine monograph.
Dose in kidney disease:
- No dosage adjustments are necessary in kidney impairment in children and adolescents from 6 to 17 years.
Levamlodipine Dose in liver disease:
- In the case of hypertension, the initial dose is typically 1.25 milligrams taken once a day.
- However, for individuals with severe liver problems, it's important to increase the dose slowly and carefully.
Common Side Effects of Levamlodipine:
- Cardiovascular:
- Edema
Less Common Side Effects of Levamlodipine:
- Cardiovascular:
- Palpitations
- Flushing
- Central nervous system:
- Fatigue
- Dizziness
- Drowsiness
- Gastrointestinal:
- Nausea
- Abdominal pain
Contraindications to Levamlodipine:
- responses due to allergies to levamlodipine, amlodipine, or any other formulation ingredient.
Warnings and precautions
Angina and myocardial Infarction
- When it comes to angina and heart attacks, there have been reports suggesting that angina or enlargement of the heart muscle may occur more often after starting treatment or changing the dose of dihydropyridine calcium channel blockers.
- Patients with a condition called obstructive cardiomyopathy might also experience rapid heartbeat, especially if they're not also taking beta-blockers at the same time.
Hypotension
- In some cases, people may experience symptoms of low blood pressure, known as hypotension.
- However, it's not very common because the decrease in blood pressure happens gradually.
- The rate at which blood pressure drops should match the patient's clinical situation.
Peripheral edema
- The most common side effect of the medication is swelling in the arms, legs, or other parts of the body, known as peripheral edema.
- This swelling might show up about 2 to 3 weeks after starting the medication.
Aortic stenosis
- Patients with severe aortic stenosis should be careful when using this medication.
- It has the potential to cause low blood pressure and decrease blood flow to the heart muscle, which could lead to a condition called ischemia.
Heart failure:
- Patients with heart failure and lower ejection fractions should avoid calcium channel blockers whenever possible.
Hepatic impairment
- Patients with liver problems should be careful when taking this medication.
- They may need to start with lower doses, and if their liver impairment is severe, they should slowly increase their dosage.
Hypertrophic cardiomyopathy and outflow tract obstruction
- Patients with hypertrophic cardiomyopathy or outflow tract obstruction should be cautious when using amlodipine because reducing the afterload (the force the heart pumps against) could worsen the symptoms of these conditions.
Levamlodipine: Drug Interaction
|
Risk Factor C (Monitor therapy) |
|
|
Alfuzosin |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Alpha1-Blockers |
The hypotensive effects of calcium channel blockers may be strengthened. |
|
Amphetamines |
may lessen the effectiveness of antihypertensive agents. |
|
Antipsychotic Agents (Second Generation [Atypical]) |
Antipsychotic drugs' hypotensive effects may be enhanced by blood pressure-lowering medications (Second Generation [Atypical]). |
|
ARIPiprazole |
ARIPiprazole's serum levels may rise in response to CYP3A4 Inhibitors (Weak). Management: Keep an eye out for enhanced pharmacologic effects of aripiprazole. Depending on the concurrent therapy and/or the indication, aripiprazole dosage modifications may or may not be necessary. For detailed advice, refer to the whole interaction monograph. |
|
Atosiban |
Calcium channel blockers may intensify Atosiban's harmful or hazardous effects. Particularly, pulmonary edoema and/or dyspnea may be at higher risk. |
|
Barbiturates |
Calcium Channel Blockers' metabolic rate could be increased. Management: Keep an eye out for any diminished therapeutic benefits of barbiturate medication when concurrently using calcium channel blockers. There may need to be dosage modifications with calcium channel blockers. The concurrent use of phenobarbital and nimodipine is not recommended. |
|
Barbiturates |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Benperidol |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Bosentan |
may reduce the serum concentration of CYP3A4 substrates (High risk with Inducers). |
|
Brigatinib |
Antihypertensive medications' potency can be decreased. Brigatinib may enhance the bradycardic activity of antihypertensive agents. |
|
Brimonidine (Topical) |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Calcium Channel Blockers (Nondihydropyridine) |
Calcium channel blockers' hypotensive effects may be exacerbated by the calcium channel blocker dihydropyridine (Nondihydropyridine). Nondihydropyridine, a calcium channel blocker, may result in a rise in serum calcium channel blocker concentration (Dihydropyridine). |
|
Calcium Salts |
may lessen the therapeutic effects of calcium channel blockers. |
|
Clopidogrel |
Calcium channel blockers may decrease the therapeutic effectiveness of clopidogrel. |
|
CycloSPORINE (Systemic) |
When calcium channel blockers (Dihydropyridine) are administered, the serum levels of cycloSPORINE may increase (Systemic). When using CycloSPORINE (Systemic), blood levels of calcium channel blockers may increase (Dihydropyridine). |
|
CYP3A4 Inducers (Moderate) |
may lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
CYP3A4 Inhibitors (Moderate) |
Levamlodipine serum levels can rise. |
|
CYP3A4 Inhibitors (Strong) |
Levamlodipine serum levels can rise. |
|
Dapoxetine |
may intensify calcium channel blockers' orthostatic hypotensive effects. |
|
Deferasirox |
may reduce the concentration of CYP3A4 substrates in serum (High risk with Inducers). |
|
Dexmethylphenidate |
can lessen an antihypertensive drug's therapeutic impact. |
|
Diazoxide |
Blood pressure-lowering medicines may strengthen their hypotensive effects. |
|
Dofetilide |
Dofetilide's serum levels may rise in the presence of CYP3A4 Inhibitors (Weak). |
|
DULoxetine |
The hypotensive impact of DULoxetine may be enhanced by blood pressure lowering medications. |
|
Efavirenz |
Calcium Channel Blockers' serum concentration can drop. |
|
Erdafitinib |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). |
|
Flibanserin |
The serum levels of Flibanserin may rise in response to CYP3A4 Inhibitors (Weak). |
|
Fluconazole |
Calcium Channel Blockers' serum levels can rise. |
|
Herbs (Hypotensive Properties) |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Hypotension-Associated Agents |
Blood pressure lowering drugs have the potential to enhance the hypotensive impact of hypotension-associated agents. |
|
Ivosidenib |
may reduce the serum concentration of CYP3A4 substrates (High risk with Inducers). |
|
Levodopa-Containing Products |
Medications that reduce blood pressure may increase the hypotensive effects of levodopa-containing products. |
|
Lormetazepam |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Lovastatin |
The serum levels of Lovastatin may rise when taken with Levamlodipine. |
|
Magnesium Salts |
Calcium channel blockers could make magnesium salts more harmful or poisonous. Calcium Channel Blockers' hypotensive effects may be strengthened by magnesium salts. |
|
Melatonin |
may reduce the effectiveness of calcium channel blockers as an antihypertensive (Dihydropyridine). |
|
Methylphenidate |
May lessen the effectiveness of antihypertensive agents. |
|
Molsidomine |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Naftopidil |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Neuromuscular-Blocking Agents (Nondepolarizing) |
The neuromuscular-blocking impact of neuromuscular-blocking agents may be enhanced by calcium channel blockers (Nondepolarizing). |
|
Nicergoline |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
Nicorandil |
Blood pressure-lowering drugs could intensify their hypotensive effects. |
|
NiMODipine |
NiMODipine's serum levels may rise in the presence of CYP3A4 Inhibitors (Weak). |
|
Nitroprusside |
Nitroprusside's hypotensive impact may be strengthened by blood pressure-lowering medications. |
|
Pentoxifylline |
Blood pressure-lowering medicines may strengthen their hypotensive effects. |
|
Pholcodine |
Pholcodine's hypotensive impact may be strengthened by blood pressure lowering medications. |
|
Phosphodiesterase 5 Inhibitors |
The hypotensive effects of blood pressure-lowering medications may be strengthened. |
|
Prostacyclin Analogues |
Blood pressure-lowering medicines may strengthen their hypotensive effects. |
|
Quinagolide |
Blood pressure-lowering medicines may strengthen their hypotensive effects |
|
QuiNIDine |
Calcium channel blockers may reduce the level of quiNIDine in the blood (Dihydropyridine). Calcium channel blockers may cause an increase in the blood levels of quinidine (Dihydropyridine). In response to quinine, blood levels of calcium channel blockers may increase (Dihydropyridine). |
|
Sarilumab |
may reduce the concentration of CYP3A4 substrates in serum (High risk with Inducers) |
|
Siltuximab |
could reduce the serum concentration of CYP3A4 substrates (High risk with Inducers). |
|
Tacrolimus (Systemic) |
Tacrolimus serum levels may rise when Calcium Channel Blockers (Dihydropyridine) are used (Systemic). |
|
Tocilizumab |
Could reduce the serum concentration of CYP3A4 substrates (High risk with Inducers). |
|
Yohimbine |
may make antihypertensive medications less effective. |
|
Risk Factor D (Consider therapy modification) |
|
|
Amifostine |
Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. |
|
Antifungal Agents (Azole Derivatives, Systemic) |
Calcium Channel Blockers' harmful or toxic effects might be exacerbated. In particular, itraconazole may make verapamil or diltiazem's unfavourable inotropic effects worse. Calcium Channel Blockers' metabolism may be slowed down by antifungal agents (systemic azole derivatives). Fluconazole and isavuconazonium, which are covered in different monographs, probably have less powerful effects than those of other azoles. Treatment: Itraconazole should not be used concurrently with felodipine or nisoldipine. With any such combination, regular monitoring is advised; calcium channel blocker dose decreases could be necessary. Fluconazole and isavuconazonium sulphate are exceptions. |
|
CarBAMazepine |
Calcium Channel Blockers' metabolism might be accelerated (Dihydropyridine). In individuals taking concurrent carbamazepine, consider adjusting the dosage of calcium channel blockers (CCBs) or switching to an alternative form of treatment. The Canadian labelling for nimodipine expressly forbids using it alongside carbamazepine. |
|
Cimetidine |
Calcium Channel Blockers' serum levels can rise. Management: Take cimetidine substitutes into consideration. If there is no acceptable substitute, watch for increased calcium channel blocker effects after starting or increasing the dosage of cimetidine and decreased effects after stopping or decreasing the dosage. |
|
CYP3A4 Inducers (Strong) |
may speed up CYP3A4 substrate metabolism (High risk with Inducers). Management: Take into account a substitute for one of the interfering medications. Specific contraindications may apply to some combinations. the relevant manufacturer's label. |
|
Dabrafenib |
may lower the serum level of CYP3A4 substrates (High risk with Inducers). Management: When feasible, look for substitutes for the CYP3A4 substrate. If concurrent therapy cannot be avoided, pay special attention to the substrate's clinical consequences (particularly therapeutic effects). |
|
Enzalutamide |
May lower the serum level of CYP3A4 substrates (High risk with Inducers). Treatment: Enzalutamide should not be used concurrently with CYP3A4 substrates that have a limited therapeutic index. Enzalutamide use, like with the use of any other CYP3A4 substrate, should be done cautiously and under close observation. |
|
Fosphenytoin |
Calcium channel blockers may raise the level of fosphenytoin in the blood. Monitoring for phenytoin toxicity while using a calcium channel blocker (CCB) at the same time or reduced phenytoin effects while stopping the CCB are the two management options. Check for diminished therapeutic effects of CCB. The Canadian labelling for nimodipine specifically forbids the use of phenytoin. |
|
Lemborexant |
Lemborexant's serum levels may rise in the presence of CYP3A4 Inhibitors (Weak). Management: When used in conjunction with weak CYP3A4 inhibitors, a maximum daily dose of 5 mg of lemborexant is advised. |
|
Lomitapide |
The blood levels of lomitapide may rise in the presence of CYP3A4 Inhibitors (Weak). Treatment: Patients taking 5 mg/day of lomitapide may continue doing so. Patients using 10 mg or more of lomitapide per day should cut their dosage in half. Maximum adult dosage of 30 mg/day may then be reached by titrating the lomitapide dose. |
|
Lorlatinib |
may lower the serum level of CYP3A4 substrates (High risk with Inducers). Management: Avoid using lorlatinib at the same time as any CYP3A4 substrates for which even a small drop in blood levels of the substrate might result in therapeutic failure and negative clinical outcomes. |
|
Macrolide Antibiotics |
Calcium Channel Blockers' metabolic rate could be decreased. Use a noninteracting macrolide as a possible management strategy. The Canadian labelling for felodipine expressly advises against using it in conjunction with clarithromycin. Azithromycin (Systemic), Fidaxomicin, Roxithromycin, and Spiramycin are exceptions. |
|
Mitotane |
May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. |
|
Obinutuzumab |
May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. |
|
Phenytoin |
The blood levels of phenytoin may rise when calcium channel blockers are used. Calcium Channel Blockers' serum levels may be reduced by phenytoin. Avoid combining nimodipine or nifedipine with phenytoin for management. With any concurrent usage, keep an eye out for phenytoin toxicity and/or diminished calcium channel blocker effects. |
|
Rifamycin Derivatives |
Calcium Channel Blockers' serum concentration can drop. This predominantly affects calcium channel blockers used orally. Management: Using rifampin with certain calcium channel blockers is not advised according to the labelling in the US and Canada. Look up the relevant labels. |
|
Simvastatin |
Simvastatin's serum levels might rise as a result of levamlodipine. Management: When at all feasible, refrain from taking simvastatin and amlodipine together. If combined, stay away from simvastatin dosages higher than 20 mg per day (for adults). |
|
Sincalide |
The therapeutic benefit of Sincalide may be reduced by medications that affect gallbladder function. Prior to using sincalide to induce gallbladder contraction, you should think about stopping any medications that can impair gallbladder motility. |
|
Triazolam |
Triazolam's serum levels may rise in the presence of CYP3A4 Inhibitors (Weak). Management: If a patient is using a concurrent mild CYP3A4 inhibitor, consider reducing the dosage of triazolam. |
|
Ubrogepant |
It's possible that CYP3A4 Inhibitors (Weak) will raise the level of ubrogepant in the blood. Treatment: The initial and second doses of ubrogepant in patients using mild CYP3A4 inhibitors should be no more than 50 mg each. |
|
Risk Factor X (Avoid combination) |
|
|
Bromperidol |
The hypotensive impact of bromperidol may be enhanced by blood pressure lowering medications. Blood Pressure Lowering Agents' hypotensive effects may be lessened by bromperidol. |
|
Pimozide |
Pimozide's serum levels may rise in response to CYP3A4 Inhibitors (Weak). |
Monitoring parameters:
Monitor Heart Rate and Blood Pressure
High Blood Pressure in Adults:
- According to the 2017 Guideline for the Prevention, Detection, Evaluation, and Management:
- If the 10-year risk of atherosclerotic cardiovascular disease is 10% or there's confirmed hypertension with a history of cardiovascular disease, the recommended target blood pressure is 130/80 mm Hg.
- For confirmed hypertension without signs of elevated risk of atherosclerotic cardiovascular disease, the recommended target blood pressure is also 130/80 mm Hg.
Diabetes and Hypertension:
- Following the American Diabetes Association guidelines:
- For patients aged 18 to 65 with a 10-year risk of atherosclerotic cardiovascular disease of less than 15% and without atherosclerotic cardiovascular disease, maintaining a target blood pressure of 140/90 mm Hg is advised.
- If they have known atherosclerotic cardiovascular disease or a 10% risk in the next ten years, a target blood pressure of 130/80 mm Hg may be recommended if it's safe.
- For patients over 65 years old:
- In good, complicated, or mediocre health, maintaining a target blood pressure of 140/90 mm Hg is advised.
- In very complex or poor health, a target blood pressure of 150/90 mm Hg is advised.
How to administer Levamlodipine?
- It may be taken once daily without regard to meals.
Mechanism of action of Levamlodipine:
- Amlodipine, a type of medication called a dihydropyridine calcium-channel blocker, works quickly on blood vessels and smooth muscles, which helps lower blood pressure by reducing resistance in the body's arteries.
- It does this by blocking the entry of calcium ions into cells, particularly in the smooth muscle cells of blood vessels.
- While it's less effective in heart muscle cells, amlodipine is still potent in treating high blood pressure.
- It's made up of both levamlodipine and dextro-amlodipine, with levamlodipine being the active form responsible for its blood pressure-lowering effects.
Protein Binding:
- Approximately 93% of the drug binds to proteins in the blood.
Onset:
- The drug's effects begin gradually.
Duration:
- The duration of action can be less than or more than 24 hours.
Excretion:
- Amlodipine is primarily excreted through urine, with about 10% of the total dose being unchanged drug and 60% as metabolites.
Metabolism:
- The liver metabolizes about 90% of the drug into inactive forms.
Half-life Elimination:
- Terminal (biphasic): Approximately 30 to 50 hours, with longer times if there's liver dysfunction.
Bioavailability:
- Amlodipine's bioavailability ranges from 64% to 90%.
Time to Peak:
- It takes about 6 to 12 hours for the drug to reach its peak concentration in the blood.
Clearance:
- The drug's clearance might be reduced in patients with liver insufficiency or moderate to severe heart failure.
- In children over 6 years old, clearance is similar to that of adults, adjusted for weight.
Levamlodipine Brand Names (International):
- S-Ambes
- Conjupri
Levamlodipine Brand Names in Pakistan:
No Brands Available in Pakistan.