Ibuprofen: Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) used primarily to relieve pain, reduce inflammation, and lower fever. It's commonly used for conditions like headaches, muscle aches, menstrual cramps, arthritis, and minor injuries. Ibuprofen works by inhibiting the production of prostaglandins, chemicals in the body that contribute to inflammation and pain.
Diphenhydramine: Diphenhydramine is an antihistamine primarily used to relieve symptoms of allergies, hay fever, and the common cold, such as sneezing, runny nose, itching, and watery eyes. It is also used as a sleep aid due to its sedative effects. Diphenhydramine works by blocking the action of histamine, a substance in the body that causes allergic symptoms.
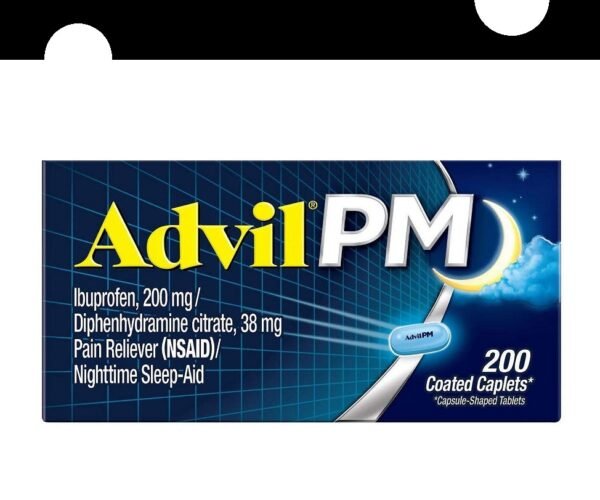
Advil PM (Ibuprofen and diphenhydramine) is a combination of an NSAID and antihistamine. It is used to relieve pain, fever, inflammation that may cause insomnia or disturbs the patient's sleep.
Advil PM (Ibuprofen and diphenhydramine) Uses:
- Insomnia and pain:
- It is used in patients with minor aches and pains that result in insomnia or the patient does not achieve an adequate full night's sleep.
Advil PM (Ibuprofen and diphenhydramine) Dose in Adults:
Advil PM (Ibuprofen and diphenhydramine) Dose in the treatment of Insomnia and pain:
- Diphenhydramine citrate 38 mg and ibuprofen 200 mg per caplet: Take two of these caplets at bedtime. Don't take more than two caplets within 24 hours.
- Diphenhydramine hydrochloride 25 mg and ibuprofen 200 mg per capsule: Take two of these capsules at bedtime. Don't take more than two capsules within 24 hours.
Remember, it's essential to follow the dosage instructions carefully and not to take more than the recommended amount within a 24-hour period.
Advil PM (Ibuprofen and diphenhydramine) dose in children:
- It should be avoided in children younger than 12 years of age.
- Doses may be given as adults, however, in young children, the maximum dose should not exceed 10 mg/kg per dose of ibuprofen or 400 mg per dose of ibuprofen (or 40 mg/kg per day of ibuprofen).
Ibuprofen and diphenhydramine Pregnancy Category: C/D
See individual agents for detailed dosing regarding its use during pregnancy and lactation:
Dose in Kidney Disease:
- The manufacturer's instructions don't mention any changes in dosage for people with kidney problems.
- This means that if you have kidney issues, you should still follow the regular dosage instructions given on the label.
Dose in Liver disease:
- The manufacturer's instructions don't mention any changes in dosage for people with liver problems.
- So, if you have liver issues, you should follow the regular dosage instructions given on the label.
Side effects of Advil PM (Ibuprofen and diphenhydramine):
See individual agents here:
Contraindications to Advil PM (Ibuprofen and diphenhydramine):
- If you're allergic to diphenhydramine, ibuprofen, any other pain reliever or fever reducer, or any ingredient in the medication, you should avoid taking it.
- Additionally, if you're experiencing perioperative pain following coronary artery bypass graft (CABG) surgery, this medication isn't suitable for you.
- It's also important to avoid using this medication simultaneously with other diphenhydramine products, including topical treatments.
- Lastly, this medication shouldn't be given to children under 12 years of age.
Warnings/Precautions
Anaphylactoid reactions
- Anaphylactoid reactions, which are severe allergic-like reactions, can occur even in patients who haven't been previously exposed to the medication.
- Patients with a condition known as the "aspirin triad," which includes bronchial asthma, aspirin intolerance, and rhinitis, may be at a higher risk of experiencing these reactions.
- It's important not to use this medication in patients who have bronchospasm, asthma, rhinitis, or urticaria (hives) when taking nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin.
- If you have any of these conditions, consult your healthcare provider before taking this medication or any NSAID.
Cardiovascular events:
- NSAIDs like ibuprofen have been linked to a higher risk of adverse cardiovascular events.
- They might also interfere with the protective effects of aspirin on the heart.
- Therefore, it's essential to use NSAIDs cautiously, especially if you have a history of cardiovascular issues.
CNS depression:
- This medication can cause central nervous system (CNS) depression, which may affect your ability to think clearly or perform tasks that require mental alertness, such as driving or operating machinery.
- It's crucial to be cautious and aware of how the medication affects you.
- Avoid engaging in activities that require concentration and quick reflexes until you know how this medication affects you personally.
Events relating to GI:
- NSAIDs, like ibuprofen, can increase the risk of gastrointestinal (GI) issues such as irritation, inflammation, ulcers, bleeding, and perforation.
- It's important to be cautious if you have a history of GI disease (like bleeding or ulcers), if you're taking aspirin, anticoagulants, or corticosteroids simultaneously, if you smoke, if you consume alcohol regularly (especially three or more drinks per day), or if you're elderly or debilitated.
- For patients with a history of acute lower GI bleeding, it's best to avoid non-aspirin NSAIDs, especially if the bleeding is due to conditions like angioectasia or diverticulosis.
Reactions to skin:
- NSAIDs, including ibuprofen, can sometimes lead to serious skin reactions.
- If you notice any signs of a skin rash or hypersensitivity, it's crucial to stop taking the medication immediately and seek medical attention.
- These skin reactions can be severe, so it's essential to act promptly if you experience any unusual skin symptoms while taking NSAIDs.
Aseptic meningitis
- Ibuprofen use may elevate the risk of aseptic meningitis, particularly in individuals with systemic lupus erythematosus (SLE) or mixed connective tissue disorders.
- It's crucial for individuals with these conditions to be cautious when using ibuprofen and to promptly report any symptoms of meningitis, such as severe headaches, fever, stiffness in the neck, or sensitivity to light, to their healthcare provider.
- If you have SLE or a connective tissue disorder, consult your healthcare provider before using ibuprofen or any NSAID.
Asthma
- It's important not to give ibuprofen to patients who have aspirin-sensitive asthma, as it may lead to severe bronchospasm.
- Even in patients with other forms of asthma, caution should be exercised when using ibuprofen.
Bariatric surgery
- After bariatric surgery, it's advised to avoid long-term use of oral nonselective NSAIDs due to the risk of gastric ulceration.
- Prolonged use can lead to the development of ulcerations or perforations in the surgical site.
- Instead, short-term use of medications like celecoxib or intravenous ketorolac is recommended as part of a multimodal pain management approach for postoperative pain.
Cardiovascular disease
- Patients with cardiovascular disease should use ibuprofen cautiously.
- It's advisable to use the lowest effective dose for the shortest duration possible to minimize the risk of cardiovascular events.
- NSAIDs like ibuprofen may also lead to fluid retention, so patients taking diuretics should exercise caution.
- Avoid using ibuprofen in individuals with heart failure.
Glaucoma and increased intraocular pressure:
- Ibuprofen should be used cautiously in patients with increased intraocular pressure or angle-closure glaucoma.
Hepatic impairment
- It's important to exercise caution when using ibuprofen in patients with decreased liver function or hepatic impairment.
- Since the liver plays a crucial role in metabolizing medications like ibuprofen, individuals with liver issues may experience altered drug metabolism and potentially increased risk of adverse effects.
Hypertension:
- Individuals with hypertension should use ibuprofen with caution because NSAIDs can potentially cause new-onset hypertension or exacerbate existing hypertension.
- Additionally, the effectiveness of medications like ACE inhibitors, thiazides, or loop diuretics may be diminished when taken alongside NSAIDs.
Prostatic hyperplasia/urinary block:
- Patients with prostatic hyperplasia (enlarged prostate) or urinary obstruction should use ibuprofen cautiously.
- NSAIDs like ibuprofen can potentially exacerbate urinary symptoms in these individuals.
Occlusion of the pyloroduodenum:
- Patients with pyloroduodenal obstruction, including stenotic peptic ulcer, should use ibuprofen cautiously.
- NSAIDs like ibuprofen can potentially exacerbate these conditions or cause complications.
Renal impairment
- Patients with renal impairment should use ibuprofen cautiously.
- NSAIDs like ibuprofen can potentially worsen existing renal function or cause complications in individuals with kidney problems.
Respiratory disease
- Patients with respiratory diseases such as emphysema or chronic bronchitis should use ibuprofen with caution.
- NSAIDs like ibuprofen can potentially exacerbate respiratory symptoms or cause complications in individuals with these conditions
Thyroid dysfunction:
- Patients with thyroid dysfunction should use ibuprofen with caution.
- While ibuprofen is generally considered safe for individuals with thyroid disorders, it's important to be cautious because NSAIDs like ibuprofen can potentially affect thyroid function or interact with medications used to treat thyroid conditions.
Ibuprofen and diphenhydramine: Drug Interaction
|
Risk Factor C (Monitor therapy) |
|
|
5-Aminosalicylic Acid Derivatives |
Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of 5-Aminosalicylic Acid Derivatives. |
|
Acalabrutinib |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Acetylcholinesterase Inhibitors |
May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. |
|
Alcohol (Ethyl) |
CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). |
|
Alcohol (Ethyl) |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the risk of GI bleeding may be increased with this combination. |
|
Aliskiren |
Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Aliskiren. Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Aliskiren. Management: Monitor renal function periodically in patients receiving aliskiren and any nonsteroidal anti-inflammatory agent. Patients at elevated risk of renal dysfunction include those who are elderly, are volume depleted, or have pre-existing renal dysfunction. |
|
Alizapride |
May enhance the CNS depressant effect of CNS Depressants. |
|
Amantadine |
May enhance the anticholinergic effect of Anticholinergic Agents. |
|
Amezinium |
Antihistamines may enhance the stimulatory effect of Amezinium. |
|
Aminoglycosides |
Nonsteroidal Anti-Inflammatory Agents may decrease the excretion of Aminoglycosides. Data only in premature infants. |
|
Aminolevulinic Acid (Topical) |
Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). |
|
Amphetamines |
May diminish the sedative effect of Antihistamines. |
|
Angiotensin II Receptor Blockers |
May enhance the adverse/toxic effect of Nonsteroidal AntiInflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Angiotensin II Receptor Blockers. The combination of these two agents may also significantly decrease glomerular filtration and renal function. |
|
Angiotensin-Converting Enzyme Inhibitors |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. |
|
Anticholinergic Agents |
May enhance the adverse/toxic effect of other Anticholinergic Agents. |
|
Anticoagulants |
Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. |
|
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.) |
May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. |
|
ARIPiprazole |
CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. |
|
Beta-Blockers |
Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. |
|
Betahistine |
Antihistamines may diminish the therapeutic effect of Betahistine. |
|
Bisphosphonate Derivatives |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Bisphosphonate Derivatives. Both an increased risk of gastrointestinal ulceration and an increased risk of nephrotoxicity are of concern. |
|
Botulinum Toxin-Containing Products |
May enhance the anticholinergic effect of Anticholinergic Agents. |
|
Brexanolone |
CNS Depressants may enhance the CNS depressant effect of Brexanolone. |
|
Brimonidine (Topical) |
May enhance the CNS depressant effect of CNS Depressants. |
|
Bromopride |
May enhance the CNS depressant effect of CNS Depressants. |
|
Cannabidiol |
May enhance the CNS depressant effect of CNS Depressants. |
|
Cannabis |
May enhance the CNS depressant effect of CNS Depressants. |
|
Cephalothin |
Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. |
|
Chloral Betaine |
May enhance the adverse/toxic effect of Anticholinergic Agents. |
|
Chlorphenesin Carbamate |
May enhance the adverse/toxic effect of CNS Depressants. |
|
CNS Depressants |
May enhance the adverse/toxic effect of other CNS Depressants. |
|
Collagenase (Systemic) |
Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. |
|
Corticosteroids (Systemic) |
May enhance the adverse/toxic effect of Nonsteroidal AntiInflammatory Agents (Nonselective). |
|
Dasatinib |
May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. |
|
Deferasirox |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. |
|
Deoxycholic Acid |
Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. |
|
Desmopressin |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Desmopressin. |
|
Dichlorphenamide |
OAT1/3 Inhibitors may increase the serum concentration of Dichlorphenamide. |
|
Digoxin |
Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Digoxin. |
|
Dimethindene (Topical) |
May enhance the CNS depressant effect of CNS Depressants. |
|
Doxylamine |
May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. |
|
Dronabinol |
May enhance the CNS depressant effect of CNS Depressants. |
|
Drospirenone |
Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Drospirenone. |
|
Eplerenone |
Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Eplerenone. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Eplerenone. |
|
Esketamine |
May enhance the CNS depressant effect of CNS Depressants. |
|
Fat Emulsion (Fish Oil Based) |
May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. |
|
Felbinac |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Gastrointestinal Agents (Prokinetic) |
Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). |
|
Glucagon |
Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. |
|
Glucosamine |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Haloperidol |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Haloperidol. Specifically including drowsiness and confusion. |
|
HydrALAZINE |
Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of HydrALAZINE. |
|
HydrOXYzine |
May enhance the CNS depressant effect of CNS Depressants. |
|
Ibritumomab Tiuxetan |
Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. |
|
Ibrutinib |
May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. |
|
Inotersen |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Itopride |
Anticholinergic Agents may diminish the therapeutic effect of Itopride. |
|
Kava Kava |
May enhance the adverse/toxic effect of CNS Depressants. |
|
Limaprost |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Lofexidine |
May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. |
|
Lumacaftor |
May decrease the serum concentration of Ibuprofen. |
|
Magnesium Sulfate |
May enhance the CNS depressant effect of CNS Depressants. |
|
MetFORMIN |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of MetFORMIN. |
|
MetyroSINE |
CNS Depressants may enhance the sedative effect of MetyroSINE. |
|
Mianserin |
May enhance the anticholinergic effect of Anticholinergic Agents. |
|
Minocycline (Systemic) |
May enhance the CNS depressant effect of CNS Depressants. |
|
Mirabegron |
Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. |
|
Multivitamins/Fluoride (with ADE) |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Multivitamins/Minerals (with ADEK, Folate, Iron) |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Multivitamins/Minerals (with AE, No Iron) |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Nabilone |
May enhance the CNS depressant effect of CNS Depressants. |
|
Naftazone |
May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Nitroglycerin |
Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. |
|
Obinutuzumab |
Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. |
|
Omega-3 Fatty Acids |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Pentosan Polysulfate Sodium |
May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. |
|
Pentoxifylline |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Perhexiline |
CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. |
|
Piribedil |
CNS Depressants may enhance the CNS depressant effect of Piribedil. |
|
Porfimer |
Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. |
|
Potassium-Sparing Diuretics |
Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Potassium-Sparing Diuretics. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. |
|
PRALAtrexate |
Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of PRALAtrexate. More specifically, NSAIDS may decrease the renal excretion of pralatrexate. Management: Closely monitor for increased pralatrexate serum levels and/or toxicity if used concomitantly with an NSAID. Monitor for decreased pralatrexate serum levels with NSAID discontinuation. |
|
Pramipexole |
CNS Depressants may enhance the sedative effect of Pramipexole. |
|
Probenecid |
May increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. |
|
Prostacyclin Analogues |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Prostaglandins (Ophthalmic) |
Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Prostaglandins (Ophthalmic). Nonsteroidal Anti-Inflammatory Agents may also enhance the therapeutic effects of Prostaglandins (Ophthalmic). |
|
Quinolones |
Nonsteroidal Anti-Inflammatory Agents may enhance the neuroexcitatory and/or seizure-potentiating effect of Quinolones. Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Quinolones. |
|
Ramosetron |
Anticholinergic Agents may enhance the constipating effect of Ramosetron. |
|
ROPINIRole |
CNS Depressants may enhance the sedative effect of ROPINIRole. |
|
Rotigotine |
CNS Depressants may enhance the sedative effect of Rotigotine. |
|
Rufinamide |
May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. |
|
Salicylates |
Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. |
|
Tacrolimus (Systemic) |
Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Tacrolimus (Systemic). |
|
Tetrahydrocannabinol |
May enhance the CNS depressant effect of CNS Depressants. |
|
Tetrahydrocannabinol and Cannabidiol |
May enhance the CNS depressant effect of CNS Depressants. |
|
Thiazide and Thiazide-Like Diuretics |
May enhance the nephrotoxic effect of Nonsteroidal AntiInflammatory Agents. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Thiazide and Thiazide-Like Diuretics. |
|
Thiazide and Thiazide-Like Diuretics |
Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. |
|
Thrombolytic Agents |
Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. |
|
Tipranavir |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Tolperisone |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Tolperisone. Specifically, the risk of hypersensitivity reactions may be increased. Tolperisone may enhance the therapeutic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Topiramate |
Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. |
|
Tricyclic Antidepressants (Tertiary Amine) |
May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). |
|
Trimeprazine |
May enhance the CNS depressant effect of CNS Depressants. |
|
Vancomycin |
Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Vancomycin. |
|
Verteporfin |
Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. |
|
Vitamin E (Systemic) |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Voriconazole |
May increase the serum concentration of Ibuprofen. Specifically, concentrations of the S-(+)-ibuprofen enantiomer may be increased. |
|
Zanubrutinib |
May enhance the antiplatelet effect of Agents with Antiplatelet Properties. |
|
Risk Factor D (Consider therapy modification) |
|
|
Apixaban |
Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Apixaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of apixaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. |
|
Bemiparin |
|
|
Bemiparin |
Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. |
|
Benzylpenicilloyl Polylysine |
Antihistamines may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Suspend systemic H1 antagonists for benzylpenicilloyl-polylysine skin testing and delay testing until systemic antihistaminic effects have dissipated. A histamine skin test may be used to assess persistent antihistaminic effects. |
|
Bile Acid Sequestrants |
May decrease the absorption of Nonsteroidal Anti-Inflammatory Agents. |
|
Blonanserin |
CNS Depressants may enhance the CNS depressant effect of Blonanserin. |
|
Buprenorphine |
CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. |
|
Chlormethiazole |
May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. |
|
CycloSPORINE (Systemic) |
Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of CycloSPORINE (Systemic). Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. Management: Consider alternatives to nonsteroidal anti-inflammatory agents (NSAIDs). Monitor for evidence of nephrotoxicity, as well as increased serum cyclosporine concentrations and systemic effects (eg, hypertension) during concomitant therapy with NSAIDs. |
|
Dabigatran Etexilate |
Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of dabigatran and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. |
|
Diclofenac (Systemic) |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Management: Seek alternatives to the combined use of diclofenac with other nonsteroidal anti-inflammatory agents (NSAIDs). Avoid the use of diclofenac/misoprostol with other NSAIDs. |
|
Droperidol |
May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. |
|
Edoxaban |
Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of edoxaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. |
|
Enoxaparin |
Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue nonsteroidal anti-inflammatory agents (NSAIDs) prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. |
|
Enoxaparin |
Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. |
|
Flunitrazepam |
CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. |
|
Heparin |
Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or nonsteroidal anti-inflammatory agents (NSAIDs) if coadministration is required. |
|
Heparin |
Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. |
|
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry) |
May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. |
|
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry) |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Bleeding may occur. Management: Concomitant treatment with these agents should generally be avoided. If used concomitantly, increased diligence in monitoring for adverse effects (eg, bleeding, bruising, altered mental status due to CNS bleeds) must be employed. |
|
Hyaluronidase |
Antihistamines may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving antihistamines (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. |
|
HYDROcodone |
CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. |
|
Imatinib |
Ibuprofen may decrease the serum concentration of Imatinib. Specifically, ibuprofen may decrease intracellular concentrations of imatinib, leading to decreased clinical response. Management: Consider using an alternative to ibuprofen in patients who are being treated with imatinib. Available evidence suggests other NSAIDs do not interact in a similar manner. |
|
Lemborexant |
May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. |
|
Lithium |
Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Lithium. |
|
Loop Diuretics |
Nonsteroidal Anti-Inflammatory Agents may diminish the diuretic effect of Loop Diuretics. Loop Diuretics may enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Management: Monitor for evidence of kidney injury or decreased therapeutic effects of loop diuretics with concurrent use of an NSAID. Consider avoiding concurrent use in CHF or cirrhosis. Concomitant use of bumetanide with indomethacin is not recommended. |
|
Methotrexate |
Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Methotrexate. Management: Alternative anti-inflammatory therapy should be considered whenever possible, especially if the patient is receiving higher, antineoplastic doses of methotrexate. |
|
Methotrimeprazine |
CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. |
|
Opioid Agonists |
CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. |
|
OxyCODONE |
CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. |
|
PEMEtrexed |
Ibuprofen may increase the serum concentration of PEMEtrexed. Management: In patients with an estimated creatinine clearance of 45 to 79 mL/min, avoid ibuprofen for 2 days before, the day of, and 2 days following the administration of pemetrexed. Monitor for increased pemetrexed toxicities if combined. |
|
Perampanel |
May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. |
|
Pramlintide |
May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. |
|
Rivaroxaban |
Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of rivaroxaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. |
|
Salicylates |
Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Salicylates. An increased risk of bleeding may be associated with use of this combination. Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the cardioprotective effect of Salicylates. Salicylates may decrease the serum concentration of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Exceptions: Choline Magnesium Trisalicylate. |
|
Secretin |
Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. |
|
Selective Serotonin Reuptake Inhibitors |
May enhance the antiplatelet effect of Nonsteroidal AntiInflammatory Agents (Nonselective). Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Management: Consider alternatives to NSAIDs. Monitor for evidence of bleeding and diminished antidepressant effects. It is unclear whether COX-2-selective NSAIDs reduce risk. |
|
Serotonin/Norepinephrine Reuptake Inhibitors |
May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). |
|
Sincalide |
Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. |
|
Sodium Oxybate |
May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. |
|
Sodium Phosphates |
May enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with NSAIDs, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, maintain adequate hydration and monitor renal function closely. |
|
Suvorexant |
CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. |
|
Tapentadol |
May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. |
|
Tenofovir Products |
Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Tenofovir Products. Management: Seek alternatives to these combinations whenever possible. Avoid use of tenofovir with multiple NSAIDs or any NSAID given at a high dose. |
|
Vitamin K Antagonists (eg, warfarin) |
Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the anticoagulant effect of Vitamin K Antagonists. Management: Consider alternatives to this combination when possible. If the combination must be used, monitor coagulation status closely and advise patients to promptly report any evidence of bleeding or bruising. |
|
Zolpidem |
CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. |
|
Risk Factor X (Avoid combination) |
|
|
Acemetacin |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Aclidinium |
May enhance the anticholinergic effect of Anticholinergic Agents. |
|
Aminolevulinic Acid (Systemic) |
Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). |
|
Azelastine (Nasal) |
CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). |
|
Bromperidol |
May enhance the CNS depressant effect of CNS Depressants. |
|
Cimetropium |
Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. |
|
Dexibuprofen |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Dexibuprofen. |
|
Dexketoprofen |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Eluxadoline |
Anticholinergic Agents may enhance the constipating effect of Eluxadoline. |
|
Floctafenine |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Glycopyrrolate (Oral Inhalation) |
Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). |
|
Glycopyrronium (Topical) |
May enhance the anticholinergic effect of Anticholinergic Agents. |
|
Ipratropium (Oral Inhalation) |
May enhance the anticholinergic effect of Anticholinergic Agents. |
|
Ketorolac (Nasal) |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Ketorolac (Systemic) |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Levosulpiride |
Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. |
|
Macimorelin |
Nonsteroidal Anti-Inflammatory Agents may diminish the diagnostic effect of Macimorelin. |
|
Mifamurtide |
Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Mifamurtide. |
|
Morniflumate |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). |
|
Omacetaxine |
Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of nonsteroidal antiinflammatory drugs (NSAIDs) with omacetaxine in patients with a platelet count of less than 50,000/uL. |
|
Orphenadrine |
CNS Depressants may enhance the CNS depressant effect of Orphenadrine. |
|
Oxatomide |
May enhance the anticholinergic effect of Anticholinergic Agents. |
|
Oxomemazine |
May enhance the CNS depressant effect of CNS Depressants. |
|
Paraldehyde |
CNS Depressants may enhance the CNS depressant effect of Paraldehyde. |
|
Pelubiprofen |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Phenylbutazone |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Pitolisant |
Antihistamines may diminish the therapeutic effect of Pitolisant. |
|
Potassium Chloride |
Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. |
|
Potassium Citrate |
Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. |
|
Revefenacin |
Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. |
|
Talniflumate |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Tenoxicam |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
|
Thalidomide |
CNS Depressants may enhance the CNS depressant effect of Thalidomide. |
|
Tiotropium |
Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. |
|
Umeclidinium |
May enhance the anticholinergic effect of Anticholinergic Agents. |
|
Urokinase |
Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. |
|
Zaltoprofen |
May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. |
Monitoring Parameters:
See how the therapy is working. Particularly in individuals who are at risk of developing renal failure, keep an eye out for kidney impairment.
How to administer Ibuprofen and diphenhydramine?
Administering with Food or Milk:
- If you experience stomach upset after taking ibuprofen, you can take it with food or milk.
- This can help reduce the chances of stomach discomfort or irritation caused by ibuprofen.
- Taking ibuprofen with food or milk is a simple way to make it easier on your stomach.
Mechanism of action of Advil PM (Ibuprofen and diphenhydramine):
- Ibuprofen, a reversible inhibitor, of the enzyme cyclooxygenase I and II, is a medication that reduces inflammation, fever, and pain.
- You can find detailed pharmacology information here.Ibuprofen (Brufen). Diphenhydramine is an antihistamine that blocks H-1 receptors.
- It blocks the release of histamine, has sedative effects and anticholinergic qualities.
- See detailed pharmacology of diphenhydramine here: Diphenhydramine (Benadryl).
International Brand Names of Ibuprofen and diphenhydramine:
- Advil PM
- GoodSense Ibuprofen PM
- Motrin PM
- Advil Night
Ibuprofen and diphenhydramine Brand Names in Pakistan:
Not Available.