A summary of the updated 2020 Asthma GINA Guidelines is presented here. This discussion includes the following topics:
- The definition of asthma
- Asthma Phenotypes
- Asthma symptoms
- Investigations to diagnose Asthma, and
- The differential diagnosis
Asthma severity assessment, asthma treatment and asthma management/ action plans will be discussed in other posts.
Introduction of Asthma GINA Guidelines - Diagnosis and Evaluation:
Asthma is a very common chronic disorder of the airways that may manifest as episodic cough, wheezing, and shortness of breath. It affects 1 - 18% of the population.
The symptoms of asthma may vary in severity depending on the individual's exposure to allergens. Asthma symptoms may spontaneously resolve for months or may become persistent especially in chronic uncontrolled asthmatics with continuous exposure to allergens.
What is Asthma?
It is a heterogeneous disease characterized by a reversible and variable airflow limitation, bronchial hyper-responsiveness, and airway inflammation. According to the National Asthma Education and Prevention Program, Asthma is defined as: "a common chronic disorder of the airways that is complex and characterized by variable and recurring symptoms, airflow obstruction, bronchial hyperresponsiveness, and an underlying inflammation.
The interaction of these features of asthma determines the clinical manifestations and severity of asthma and the response to treatment" [Ref]
As per the Asthma GINA Guidelines 2020 final report [Ref], Asthma is defined as: Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity, together with variable expiratory airflow limitation"
Asthma Phenotypes:
As mentioned above, asthma is a heterogeneous disease. This means asthmatics can be divided into two different clusters based on demographics, clinical features, and pathophysiological processes.
Occasionally, the recognition of different phenotypes can guide the physician to specific management. However, most asthma phenotypes follow the same management protocols.
Common Asthma Phenotypes are:
- Allergic Asthma or the Eosinophilic Phenotype of Asthma:
- This is the most common phenotype of asthma. Patients usually develop symptoms during their early childhood that progress as they age.
- Patients may also report other allergic symptoms suggestive of atopies such as dermatitis or eczema, rhinitis, and food allergies.
- A family history of atopic diseases or asthma may be present as well.
- The sputum of these patients may demonstrate eosinophils, hence the term, eosinophilic asthma.
- These patients best respond to inhalational corticosteroids.
- Non-allergic asthma:
- This phenotype of asthma is not secondary to atopy or allergies.
- Sputum examination of these patients may contain neutrophils, and eosinophils, or may not contain any specific cell type.
- Contrary to the allergic or eosinophilic phenotype of asthma, these patients do not respond well to inhaled corticosteroids.
- Adult-onset or Late-onset Asthma:
- Adult-onset asthma is present later in life and usually affects middle-aged women.
- It behaves as non-allergic asthma. These patients do not respond to inhalational corticosteroids and require very high doses.
- It is important to exclude the possibility of occupational asthma in this group of patients.
- Persistent Asthma:
- Persistent asthma develops in patients with long-standing uncontrolled disease.
- These patients have persistent symptoms despite therapy.
- Longstanding uncontrolled diseases cause airway remodeling that is not reversible.
- Asthma with obesity:
- Obese patients may develop airway hyper-responsiveness and symptoms of asthma.
- These patients usually do not have eosinophilic airway disease.
Other variants such as exercise-induced asthma have not been included in the list of asthma phenotypes of 2020 Asthma GINA guidelines.
Asthma GINA Guidelines - Symptoms and Signs:
The four cardinal symptoms of asthma are:
- Wheezing
- Shortness of Breath
- Cough and/or
- Chest tightness
The probability of asthma increases if:
- More than one symptom is present
- The symptoms are episodic and recur
- The symptoms vary in intensity and are worse especially at night and in the early morning.
- These symptoms are triggered by:
- Viral infections and the common cold
- Irritants such as Dust, exhaust fumes, and strong smell
- Allergen exposure (including food allergens)
- Laughter and exercise
- Changes in weather
The probability of asthma decreases in the presence of the following symptoms:
- Isolated cough without other symptoms
- Chronic sputum production
- Shortness of breath is associated with light-headedness, dizziness, and tingling and numbness of the hands.
- Chest pain
- Exercise-induced shortness of breath with noisy breathing.
It is also important to note that a childhood history of respiratory symptoms, a family history of asthma, and a history of allergic rhinitis and dermatitis may give us clues to the diagnosis of asthma, however, these features are not present in all asthma variants. Nevertheless, a history of allergic rhinitis and atopic dermatitis may be suggestive of the eosinophilic/ allergic variant of asthma.
Clinical Signs of Asthma:
Physical examination in most patients with asthma is normal. Some patients may have an audible wheeze that could be heard even without a stethoscope. Rhonchi or Rales are musical sounds that may be heard during the expiratory phase.
In mild cases, rhonchi can only be heard when the patient is asked to expire forcefully. In severe cases, as well as in very mild cases such as patients with mild intermittent asthma, no clinical signs may be present on physical examination of the chest.
"Silent Chest"is the absence of breath sounds that may be a clue to impending respiratory failure. Patients with severe asthma may have a "silent chest" along with other clinical signs of respiratory fatigue and failure.
It is important to note that crepitations and inspiratory wheeze (or Stridor) are not features of asthma. It is also important to note that "WHEEZING" is not present only in patients with asthma.
It is a sign of airflow obstruction and may be present in other conditions that result in airflow obstruction such as chronic obstructive pulmonary disease, foreign body inhalation, tracheomalacia, laryngeal obstruction, respiratory tract infections, and cardiac failure.
Asthma GINA Guidelines - Investigations in patients with Asthma:
Asthma is a clinical diagnosis, however, confirmation of the diagnosis is essential. Confirmation of asthma is particularly important in patients with atypical features such as those with late-onset asthma and non-allergic asthma.
Investigations are also important to exclude asthma mimickers such as cardiac failure, COPD, and tracheomalacia. Most patients do not need any specific test to diagnose asthma, however, the following investigations may be advised to confirm the diagnosis, and assess the severity of the disease, and comorbid conditions.
- Lung Function Tests
- Bronchial Provokation Tests
- Allergen Testing
Lung Function Tests:
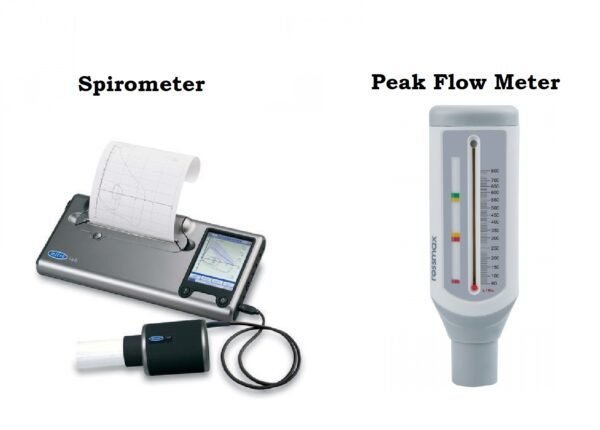
Lung function tests are performed to assess the degree of airflow limitation and reversibility after the inhalation of a bronchodilator. Two commonly used methods are used:
- Peak expiratory flow (PEF)
- Forced expiratory volume in one second (FEV-1)
Peak Expiratory Flow or PEF is a relatively easier method and can be performed at home as well. It is performed with a simple device called Peak Flow Meter. PEF is less accurate than FEV-1, however, it can be easily performed with a hand-held device at home to assess the severity of the disease by the patient. FEV-1 is performed via a spirometer.
It requires a well-trained technician and calibrated standardized equipment. It is more accurate than PEF, however, disease severity, especially in emergency situations. Two common terms are used to describe lung function tests: Variability and reversibility.
ariability means improvement or deterioration in the PEF or FEV-1 over the day, season, or course of the disease.
Reversibility or Responsiveness is the rapid improvement in pulmonary functions as measured by PEF or FEV-1 after the inhalation of a bronchodilator or improvement after a few days of inhaled corticosteroid therapy.
Documenting excessive variability is an essential component of Asthma. Excessive variability can be determined by:
- An improvement in pulmonary functions after inhaled bronchodilator therapy or after a trial of controlled treatment.
- A reduction in the pulmonary function after bronchial provocation and exercise
- Variability is demonstrated over a variable period of time as measured at different times of the day, on different days, or on separate visits over at least 1 - 2 weeks.
The greater the variation in the pulmonary function, the more likely the diagnosis of asthma. Variability can be observed in other conditions to some extent such as COPD. In general, the diagnosis of asthma is established if the person has a clinical history suggestive of asthma along with the following pulmonary function test readings:
- An increase or decrease in the FEV-1 of greater than 12% and greater than 200 ml from the baseline.
- If spirometry is not available, a change in the PEF of at least 20%.
- The average of diurnal PEF variability, calculated two times a day over 1 - 2 weeks, was greater than 10% in adults and greater than 13% in healthy children. It is calculated by the following formula:
- ([Day's highest readings - Day's lowest readings]/ average of the day's highest and lowest readings) x 100
It is better to document variability prior to initiating the treatment as variability is affected by many factors. These include:
- It decreases with the treatment as the lung functions improve
- Bronchodilator reversibility may be absent between symptoms, after beta-2 agonist therapy, in viral infections, and severe persistent asthma.
Bronchial Provocation Tests:
The bronchial provocation test (BPT) is considered sensitive but less specific. A positive BPT has little value as it may be present in other conditions such as allergic rhinitis, cystic fibrosis, COPD, or bronchopulmonary dysplasia.
However, a negative test can reliably exclude asthma, since the test is more specific. BPT is performed via different agents such as inhaled methacholine, histamine, exercise, inhaled mannitol, and eucapnic voluntary hyperventilation.
Allergy Testing:
Allergy testing has little value in the diagnosis of asthma. However, it may enable the physician to document atopy. Atopy can be assessed by measuring IgE levels in the serum or skin prick testing for common environmental allergens.
Skin prick testing is less expensive, simple, rapidly performed, and has a higher sensitivity than IgE levels. IgE level in the serum is more expensive but can be valuable in uncooperative patients, those with diffuse skin disease, and patients with a history of anaphylaxis.
FeNO (Fractional Excretion of Nitric Oxide):
Exhaled FeNO is usually higher in asthmatics characterized by type 2 airway inflammation. FeNO can also be elevated in other conditions such as eosinophilic bronchitis, atopy, allergic rhinitis, and eczema.
It may be falsely normal in patients with the neutrophilic phenotype of asthma. It may also be lower in smokers, during the early phase of allergic response, and when bronchospasm is present.
Differential Diagnosis of Asthma:
The following list of diseases may be considered in patients with symptoms of cough, shortness of breath, and chest tightness.
Age | Symptoms | Diagnosis |
| 6 – 11 years |
| Chronic upper airway cough syndrome |
| Foreign body inhalation | |
| Bronchiectasis | |
| Primary Ciliary Dyskinesia | |
| Congenital heart disease | |
| Bronchopulmonary dysplasia | |
| Cystic Fibrosis | |
| 12 – 39 years |
| Inducible laryngeal obstruction |
| Hyperventilation, dysfunctional breathing | |
| COPD | |
| bronchiectasis | |
| Cardiac failure | |
| Medication-related cough | |
| Parenchymal lung disease | |
|
| |
| Central airway obstruction | |
| All ages |
| Tuberculosis |
Asthma GINA Guidelines - Asthma Diagnosis in other Contexts:
Patients with a dry cough as the only presenting symptom:
The following diagnosis can be considered in the list of differential diagnoses in patients who present with dry cough as the only symptom:
- Post-nasal drip (chronic upper airway cough syndrome)
- Cough induced by medications such as ACE-I
- Gastroesophageal reflux disease (GERD)
- Chronic sinusitis
- Inducible laryngeal obstruction
These diseases must be differentiated from Cough-variant asthma. Cough is the only presenting symptom in these patients, however, bronchial hyper-reactivity may be present and documentation of variability is important.
Cough-variant Asthma should also be differentiated from eosinophilic bronchitis in which the patient has sputum eosinophilia but normal spirometry and airway responsiveness.
Occupational Asthma (Work-related asthma):
Occupational asthma is usually overlooked, even though, the burden of the disease may be as high as 5 - 20%. Patients get exposed to environmental antigens, allergens, and other sensitizing agents at their workplace.
A detailed history of occupation and symptoms variability during workdays and weekends should be elicited. Symptoms are usually noticed after a change in occupation or hobbies in adults who develop recent onset chest symptoms.
Sometimes, allergic rhinitis may precede occupational asthma for years. It may be difficult to diagnose occupational asthma in such cases. Documentation of airway hyper-responsiveness via lung function tests is mandatory because of the legal and socio-economic implications of the disease.
Asthma in Athletes:
Asthma in athletes should also be confirmed via lung function tests and bronchial provocation testing. Other conditions should also be considered when investigating athletes with suspected asthma. These include:
- Rhinitis
- Inducible laryngeal obstruction
- dysfunctional breathing
- Cardiac disorders, and
- Overtraining
Asthma in the elderly patients:
Elderly patients usually ignore their symptoms. They attribute their symptoms to old age, fatigue, lack of physical activity, poor fitness, accepting dyspnea as normal, and poor perception of airflow limitation.
Furthermore, the presence of co-morbid conditions usually complicates the disease. Elderly patients should always be investigated for left ventricular failure that can cause cardiac asthma.
These patients have symptoms that worsen on lying down and with exertion. Echocardiography, ECG, and BNP levels should be done to exclude the diagnosis of the left ventricular failure. History of smoking and biomass exposure should be taken. Asthma-COPD overlap disease is considered to be more common than asthma alone.
Asthma in Smokers and Ex-smokers:
Not all smokers with dyspnea or wheezing have COPD. Asthma should be excluded in these patients by appropriate investigations. GOLD (Global Strategy for Diagnosis, Management, and Prevention of COPD) defines COPD on the basis of the following three parameters:
- Chronic respiratory symptoms
- History of exposure to risk factors such as smoking
- Post-bronchodilator FEV-1/FVC of less than 70%
Significant bronchodilator reversibility may be found in patients with COPD. Compared to asthmatics, COPD patients are likely to have low diffusion capacity. Asthma-COPD Overlap has a worse prognosis and if the physician is in doubt about the diagnosis, early referral to a specialist is essential.
Asthma in Obese patients:
Although asthma is more common in obese individuals, both under-diagnosis and over-diagnosis are common. Obese individuals should have an objective assessment of bronchial hyper-responsiveness. These patients may have dyspnea due to fatigue, low exercise tolerance, GERD, and Obstructive sleep apnea.
The following table summarizes the diagnosis of asthma:
Diagnostic Feature | Criteria for making the diagnosis of asthma |
A history of variable respiratory symptoms | |
|
|
Confirm Variable expiratory airflow limitation | |
| Documented excessive variability in one or more of the tests below | The greater the variation or on more occasions the variability is seen, the more confident the diagnosis of asthma. |
| Positive bronchodilator reversibility test (SABA should be withheld for 4 hours or more, LABA should be withheld for 15 hours or more) | At a time when the FEV-1 is reduced, confirm that the FEV-1/FVC is reduced (It is usually > 0.75 – 0.80 in adults and > 0.9 in children.
|
| Excessive variability in twice-daily PEF over two weeks |
|
| Significant increase in lung function tests after 4 weeks of anti-inflammatory therapy | Adults: Increase in FEV-1 by greater than 12% and 200 ml or PEF of > 20% from baseline after four weeks of treatment (without respiratory infections) |
| Positive exercise challenge test |
|
| Positive Bronchial challenge test |
|
| Excessive variation in lung function tests between visits |
|
Asthma Severity assessment and Management as per Asthma GINA Guidelines 2020 will be posted later ... Stay Tuned!

 Injection for familial chylomicronemia syndrome.jpeg)

