Heparin Sodium injection inhibits the formation of fibrin from fibrinogen by inhibiting thrombin and other clotting factors. It is used in the prevention and treatment of arterial and venous thrombosis such as deep vein thrombosis and pulmonary embolism.
Heparin Uses:
- It is used in bladder pain syndrome leading to Interstitial cystitis.
- It is also used as a part of the management of Non-ST elevated myocardial infarction.
- As a part of management during PCI.
- ST-elevated myocardial infarction.
- Heparin is recommended as an anticoagulant in several conditions in addition to those above, such as the following, Superficial vein thrombosis, nonbacterial thrombotic endocarditis, cerebral venous sinus thrombosis, and acute arterial emboli or thrombosis. These are according to Antithrombotic guidelines from the American College of Chest Physicians. (ACCP). See the ACCP antithrombotic guidelines for more details.
Heparin Dose in Adults:
- It should be noted that dose adjustment according to the weight, the use of institution-specific dosing nomograms are recommended.
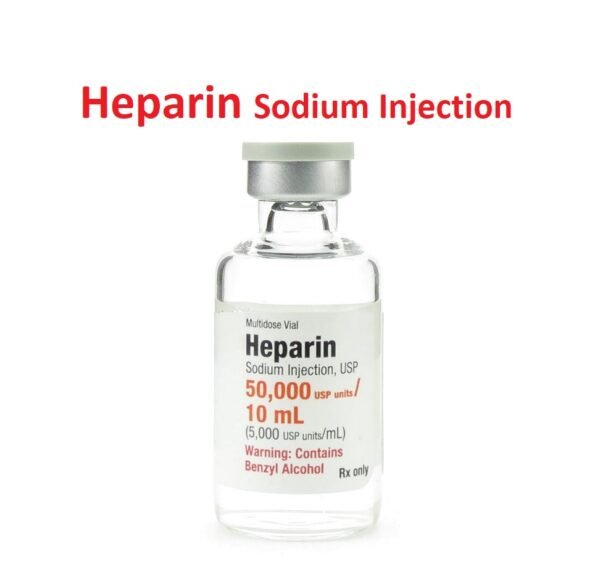
- Many concentrations of heparin are available ranging from 1 unit/mL to 20,000 units/mL.
- Carefully examine each prefilled syringe or vial before using it and ensure that the correct concentration is chosen.
- Heparin lock flush solution is intended only to maintain the patency of IV devices and is not to be used for anticoagulant therapy.
Heparin Dose in the treatment of Ischemic heart disease:
If clinically indicated, a glycoprotein (GP) IIb/IIIa inhibitor (eg, abciximab, eptifibatide, tirofiban) can be administered in combination with parenteral anticoagulation like heparin and other antiplatelet agents (eg, aspirin and a P2Y12 inhibitor [eg, clopidogrel, prasugrel, ticagrelor]) during the percutaneous coronary intervention (PCI) for ischemic heart disease. However, More bleeding complications are associated with the use of Glycoprotein IIb/IIIa inhibitors.
-
Acute coronary syndromes (ACS):
-
Heparin dose in ST-elevation myocardial infarction (STEMI) (off-label):
- Adjunct to PCI:
- No planned GP IIb/IIIa inhibitor use:
- In such cases IV Bolus of70 to 100 units/kg to achieve ACT of 250 to 300 seconds.
- The goal ACT may vary depending on point of care device.
- Re-administer as needed to maintain goal ACT throughout the procedure.
- Planned GP IIb/IIIa inhibitor use:
- IV Bolus of 50 to 70 units/kg to achieve ACT of 200 to 250 seconds regardless of point of care device.
- Readminister as needed to maintain goal ACT throughout the procedure.
- No planned GP IIb/IIIa inhibitor use:
- Adjunct to fibrinolysis (eg, full-dose alteplase, reteplase, or tenecteplase):
- It can be given as IV Bolus of 60 units/kg with maximum dose of 4,000 units, followed by 12 units/kg/hour up to maximum dose of 1,000 units/hour.
- Adjust infusion to target aPTT of 1.5 to 2 times control (~50 to 70 seconds).
- Continue for a minimum period of 48 hours or until revascularization, if performed.
- No planned reperfusion:
- Limited studies have been done. Some experts are of opinion that IV Bolus of 50 to 70 units/kg up to maximum of 5,000 units, followed by 12 units/kg/hour.
- And adjust infusion to target aPTT of 1.5 to 2 times control (~50 to 70 seconds).
- Continue for more than 48 hours.
- Adjunct to PCI:
-
-
Non-ST-elevation ACS (off-label):
-
Ischemia-guided approach:
- IV: Bolus 60 units/kg (maximum: 5,000 units), followed by 12 units/kg/hour (maximum: 1,000 units/hour); adjust infusion to target aPTT of 1.5 to 2 times control (~50 to 70 seconds).
- Recommended duration is ≥48 hours or until management changes to an invasive strategy; if PCI is performed see Percutaneous coronary intervention for dosing guidance.
-
Invasive approach (an adjunct to PCI):
- No planned GP IIb/IIIa inhibitor use:
- In invasive approach IV Bolus of 70 to 100 units/kg are given to achieve ACT of 250 to 300 seconds with goal ACT might vary depending upon point of care device.
- Readminister it as needed to maintain goal ACT throughout the procedure.
- Planned GP IIb/IIIa inhibitor use:
- An IV Bolus of 50 to 70 units/kg to achieve ACT of 200 to 250 seconds without taking into account for point of care device.
- Readminister as needed to maintain goal ACT throughout the procedure.
- No planned GP IIb/IIIa inhibitor use:
-
Heparin Dose in the treatment of Percutaneous coronary intervention (off-label):
-
No prior anticoagulant therapy:
- No planned GPIIb/IIIa inhibitor use:
- In such cases heparin can be given as an IV initial bolus of 70 to 100 units/kg to achieve ACT of 250 to 300 seconds keeping goal ACT which may vary depending on point of care device.
- Readminister it as needed to maintain goal ACT throughout procedure.
- Planned GPIIb/IIIa inhibitor use:
- An initial bolus of 50 to 70 units/kg can be given to achieve ACT of 200 to 250 seconds regardless of the point of care device used.
- Readminister heparin as needed to maintain goal ACT throughout procedure.
- No planned GPIIb/IIIa inhibitor use:
-
Prior anticoagulant therapy:
-
Prior anticoagulation with heparin:
- No planned GP IIb/IIIa inhibitor use:
- IV: Re-dose heparin as needed (eg, 2,000 to 5,000 units) to maintain goal ACT of 250 to 300 seconds throughout procedure (goal ACT may vary depending on point of care device).
- Planned GP IIb/IIIa inhibitor use:
- It can be given as IV.
- And Re-administer heparin as needed (eg, 2,000 to 5,000 units) to maintain goal ACT of 200 to 250 seconds throughout procedure (regardless of point of care device).
- No planned GP IIb/IIIa inhibitor use:
-
Prior anticoagulation with enoxaparin:
- If PCI occurs less than 12 hours after the last SubQ dose of enoxaparin.
- If PCI occurs after 12 hours after the last SubQ dose of enoxaparin then you may use an established anticoagulation regimen (eg, full-dose heparin).
-
Prior anticoagulation with fondaparinux:
- No planned GP IIb/IIIa inhibitor use:
- Then give IV Bolusof 85 units/kg to achieve ACT of 250 to 300 seconds keeping the goal ACT which may vary depending on point of care device.
- Readminister it as needed to maintain goal ACT throughout the procedure.
- Planned GP IIb/IIIa inhibitor use:
- Give IV Bolus of 60 units/kg to achieve ACT of 200 to 250 seconds regardless of point of care device.
- Readminister heparin as needed to maintain goal ACT throughout the procedure.
- No planned GP IIb/IIIa inhibitor use:
-
Heparin Dose in the treatment of Atrial fibrillation (to prevent stroke and systemic embolism):
-
General guidelines pertaining to peri-cardioversion use:
- For intravenous administration, if the patient is not on another anticoagulant prior to presentation, start heparin and titrate up based on an institutional protocol to maintain an aPTT equivalent to anti-Xa activity in the range of 0.3 to 0.7 units/mL.
-
Cardioversion:
-
Patients with atrial fibrillation >48 hours or unknown duration:
- In such cases, the patient should receive therapeutic anticoagulation (which is usually an oral anticoagulant for more than 3 weeks prior to cardioversion.
- Alternatively, a transesophageal echocardiogram (TEE) can be performed and if no thrombus is seen, cardioversion may be performed within 24 hours.
-
Patients with atrial fibrillation <48 hours:
- In such cases begin heparin at the time of presentation.
- Cardioversion may be performed without waiting for 3 weeks of anticoagulation prior to the procedure.
-
Emergency cardioversion in a hemodynamically unstable patient:
- heparin should be started at the time of presentation, but the initiation of anticoagulation should not delay emergency cardioversion.
- Cardioversion may be performed without 3 weeks of anticoagulation prior to the procedure.
- Note:
- In all scenarios, patients should be shifted to an oral anticoagulant and receive therapeutic anticoagulation for at least 4 weeks after cardioversion.
-
Heparin Dose during Cardiopulmonary bypass:
- Initially, it can be given intravenously as 300 to 400 units/kg before arterial or venous cannulation.
- Cardiopulmonary bypass may be started once ACT is at least 400 to 480 seconds depending on the instrument used.
- ACT should be measured every 30 minutes and administer additional heparin boluses as necessary.
- It is notable that an ACT of 400 is adequate for instruments using maximal activation whereas an ACT of 480 is preferred for standard instruments using a single activator.
Heparin Dose during Dialysis, anticoagulation of circuit:
-
Intermittent hemodialysis:
-
Standard dose:
- The standard dose is given initially as Bolus 2,000 units.
- Repeat bolus halfway through hemodialysis treatment or may start a continuous infusion of 500 units/hour after the initial bolus.
- Then titrate to maintain an ACT of 200 to 250 seconds throughout the procedure.
- If an infusion is given, turn off the infusion 30 minutes before the end of the procedure.
-
Minimum dose (for patients at high risk for bleeding):
- In such cases, it can be given IV as an initial bolus of 500 units repeat boluses every 30 minutes or may start a continuous infusion of 250 to 500 units/hour after the initial bolus.
- Monitor frequently and titrate to maintain an ACT of 150 to less than 200 seconds throughout the procedure.
-
-
Continuous renal replacement therapy (alternative agent):
- It can be given as an initial bolus of 500 to 1,000 units. Then followed by a continuous infusion of 500 units/hour. Titrate to maintain an aPTT of approximately 45 seconds.
It is notable that standard dosing has not yet been established. Protocols should be individualized based on coagulation abnormalities and risk for bleeding.
Heparin Dose in the treatment of Interstitial cystitis (bladder pain syndrome) (off-label): Intravesical:
Various regimens of heparin (20,000 to 50,000 units) alone or with alkalinized lidocaine (1% to 4%) have been recommended. When lidocaine and heparin are mixed, there is a risk of precipitation if proper alkalinization does not occur. Prior to administration, lidocaine stability and pH should be determined after the components have been mixed.
-
Single-dose regimen:
- Instill the combination of 50,000 units of heparin, lidocaine 200 mg, and sodium bicarbonate 420 mg in 15 mL of sterile water into the bladder via the catheter and allow it to stay for 30 minutes before draining it out.
-
Once-weekly dosing regimen:
- Prepare the combination of 20,000 units of heparin, lidocaine 4% (5 mL), and sodium bicarbonate 7% (25 mL) into an empty bladder via catheter once weekly for 3 months and allow to dwell for 30 minutes before draining.
-
Twice-weekly dosing regimen:
- Instill 25,000 units of heparin which is diluted with 5 mL of sterile water and infuse into the bladder via catheter twice a week for 3 months.
-
Maintenance of catheter patency (continuous infusion):
- For the maintenance of patency of a catheter, use heparin 2 unit/mL large volume IV solutions, which can be administered at an infusion rate of 3 mL/hour (equivalent to 6 units/hour).
- However, the rate of infusion is dependent upon age, weight, clinical condition of the patient, and procedure being employed. Do not use as a "catheter lock flush".
Heparin Dose in the treatment of venous thromboembolism (VTE):
Dose as an alternative agent in the prophylaxis of VTE:
Hospitalized medical patients with acute illness at moderate to high risk for VTE (including patients with active cancer):
-
- Subcutaneously 5,000 units every 8 to 12 hours, this is a frequency of every 12 hours has been used in cancer patients but appears to be less effective.
- The recommended duration is the length of hospitalization or until fully ambulatory.
Major non-orthopedic surgery (patients with active cancer):
-
- The regimens vary and include the following:
- In the SubQ route 5,000 units 2 to 4 hours prior to surgery, then 5,000 units every 8 hours thereafter, a frequency of every 12 hours has been used but appears to be less effective.
- OR
- SubQ, it can be given as 5,000 units every 8 to 12 hours started approximately 6 to 24 hours after surgery.
- The optimal duration of prophylaxis has not yet been established.
- It is usually given for a minimum of 7 to 10 days which can be extended for up to 4 weeks and may be reasonable in those who are undergoing major abdominal or pelvic surgery.
- The regimens vary and include the following:
Heparin dose in Non orthopedic surgery (patients without cancer):
-
- For patients with a moderate and high risk of VTE and low risk of bleeding it is recommended:
- SubQ: 5,000 units every 8 to 12 hours, with the first dose given 2 hours before surgery.
- Alternatively, you can postpone pharmacologic prophylaxis until after surgery (eg, high bleeding risk) when it is safe to initiate.
- Continue until fully ambulatory and risk of VTE has diminished (typically up to 10 days).
- For patients with a moderate and high risk of VTE and low risk of bleeding it is recommended:
Heparin Dose in Orthopedic surgery (eg, hip fracture surgery [HFS]; total hip arthroplasty [THA], or total knee arthroplasty [TKA]):
- SubQ:
- 5,000 units every 8 to 12 hours, with the first dose administered more than 12 hours preoperatively or more than 12 hours postoperatively once hemostasis has been achieved.
- The optimal duration of prophylaxis is unknown but it is usually administered for a minimum of 10 to 14 days and can be extended for up to 1 month.
- Some experts are of opinion that duration in the lower end of the range (10 to 14 days) for TKA or the higher end of the range (~30 days) for THA.
- For an extended period of prophylaxis, you may transition it to an oral anticoagulant or alternative subcutaneous anticoagulant with less frequent dosing.
Heparin Dose in Pregnancy:
Patients at high VTE risk in the antepartum or postpartum period will have their dose intensities adjusted based on bleeding complications and risks of thrombosis.
-
Prophylactic dose:
- First trimester:
- SubQ: 5,000-7,000 units per 12 hours.
- Second trimester
- SubQ: 7500-10000 units per 12 hours
- Troisième trimester
- SubQ: 10,000 units per 12 hours (reduce dosage if the aPTT rises).
- First trimester:
-
Adjusted dose (therapeutic):
-
SubQ
- 10,000 units per 12 hours. Adjust the dose to achieve an aPTT between 1.5 and 2.5 times control. This is measured six hours after injection.
- This category is reserved for patients who are at highest risk, such as those with a history of severe thrombophilia or recurrent bleeding.
- Patients receiving more than 7,500 units per 12 hours or 10,000 units each 12 hours should not be given heparin.
- Patients receiving more than 10,000 units per hour should stop taking heparin longer than 24 hours prior to delivery
- consider checking coagulation parameters (eg, aPTT) before delivery. If neuraxial anesthesia is being used, it is especially important to discontinue the procedure in a timely manner.
- It can be re-initiated within 4 to 6 hours of vaginal delivery, or 6 to 12 hours following cesarean delivery, if no significant bleeding has occurred.
- High-risk women should continue anticoagulation for at least 6 weeks after delivery.
-
Heparin Dosage for Deep vein thrombosis (DVT) and/or Pulmonary embolism
-
-
Anticoagulation initial:
- Notice:
- For patients who are hemodynamically unstable, have a high clot burden, and may require invasive procedures or thrombolysis, or who have diabetes, IV heparin is preferred for the initial treatment.
- For other patients, low-molecular weight heparin or fondaparinux may be used to start therapy.
- Inpatient IV planning requires 80 units/kg or alternatively 5,000 units. IV bolus is followed by an initial continuous IV infusion of 18 units/kg/hour, or alternatively 1,000 units/hour to maintain an anti-Xa equivalent of 0.3 to 0.7% units/mL.
-
SubQ
- It is used for patients who are unable to receive intravenous monitoring or in cases where frequent monitoring is not possible.
- Initial dose is 333 units/kg. 250 units/kg are added every 12 hours.
-
Anticoagulation long-term (maintenance).
- Unfractionated Heparin is not recommended for long-term maintenance anticoagulation.
- Alternative agents such as warfarin, warfarin, and low molecular weight hemoparin [LMWH] are preferred.
-
Transitioning between anticoagulants
-
Transferring from another anticoagulant into IV heparin
- If you need to change from a SubQ LMWH/SubQ fondaparinux therapeutic dose to a therapeutic IV heparin dose, administer IV heparin at the indicated rate 1 to 2 hours before your next dose of LMWH/fondaparinux.
- There is no need to use heparin bolus.
-
Transferring from IV Heparin to an Anticoagulant
- Transition from IV heparin to IV therapeutic dosefondaparinux:
- Stop IV heparin and begin SubQ LMWH or SubQ fondaparinux within 1 hour. You should consult your local guidelines if aPTT is outside the therapeutic range when heparin is stopped.
- Transitioning from VTE prophylaxis to therapeutic IV Heparin
- It is important to start IV heparin therapy (whose rate depends on the indication) immediately. If indicated, an IV heparin loading dose/bolus can be used.
- Transition from IV heparin therapeutic dose to IV warfarin for VTE Treatment:
- Begin warfarin treatment on the first or second day. Do not overlap IV heparin with more than 2 measurements 24 hours apart.
- Transition from IV heparin to IV warfarin for nonvalvular fibrillation
- In patients who are not at high risk of immediate thromboembolism, warfarin can be started without parenteral anticoagulant (ie, no bridging).
- Patients at high risk for immediate thromboembolism should be able to overlap with IV heparin until their INR is within therapeutic limits. Bridging may also be an option.
- Transition from IV heparin at therapeutic dose to an oral anticoagulant (DOAC).
- Stop the parenteral anticoagulant injection and start DOAC.
- It is important to follow local guidelines.
- Some DOACs, such as dabigatran or edoxaban, require five days of parenteral blood coagulation before they can be used to treat VTE.
- Transition from IV heparin to IV therapeutic dosefondaparinux:
Heparin Dose in Childrens
It is noteworthy that many concentrations of heparin are available and range from 1 to 20,000 units/mL. Carefully examine each prefilled syringe, bag, or vial prior to use to ensure that the correct concentration is chosen. Heparin lock flush solution is intended only to maintain the patency of IV devices and is not to be used for anticoagulant therapy.
Heparin prophylactic intermittent dose for central line patency:
-
Infants, Children, and Adolescents:
- When using intermittent flushes of heparin to maintain patency of single and double-lumen central catheters, various recommendations are present. Local guidelines should also be consulted.
- Capped polyvinyl chloride catheters and peripheral heparin locks require flushing more frequently (eg, every 6 to 8 hours).
- The volume of heparin flush is usually similar to the volume of the catheter (or slightly greater). The dose of heparin flush used should not approach the therapeutic unit per kg dose.
- Additional flushes should be given when stagnant blood is observed in the catheter after the catheter is used for drug or blood administration and after blood withdrawal from the catheter.
Heparin dose for anticoagulation during ECMO venoarterial (VA)/Cardiac:
Note: While used to prevent thrombosis, full anticoagulation dosing is necessary;
-
Infants, Children, and Adolescents:
- It can be given in IV form as 100 units/kg prior to ECMO cannulation followed by continuous IV heparin infusion to maintain the ACT between 180 and 220 seconds. ACT should be checked hourly while the patient is on ECMO.
- Further monitoring targets for heparin therapy are prolongation of the PTT to 1.5 to 2.5 times the control value or an anti-Xa level of 0.3 to 0.7 units/mL.
Heparin dose for the patency of venous access in patients on parenteral nutrition (PN):
-
Infants, Children, and Adolescents:
- It can be given in the formulation of 1 unit/mL (final heparin concentration in PN), both central and peripheral.
- The final concentration of heparin used for PN solutions may need to be decreased to 0.5 units/mL in small infants receiving larger PN volumes in order to avoid approaching therapeutic amounts.
-
Peripheral arterial catheters in situ:
-
Infants and Children:
- Intra-arterial (via arterial catheter): Continuous infusion of heparin at a final concentration of 5 units/mL at 1 mL/hour.
-
-
Thromboprophylaxis in CHD patients with systemic to pulmonary artery shunts (eg, Sano shunt, Blalock-Taussig shunt, central shunt) or central venous lines in certain CHD patients (eg, previous thrombosis or hypercoagulable states):
-
Infants, Children, and Adolescents:
- It should be given in low doses and in continuous IV infusion i.e. 10 to 15 units/kg/hour.
-
Heparin treatment dose in Thrombosis:
-
Systemic heparinization:
-
Infants:
- In IV form the initial loading dose is 75 units/kg over 10 minutes. Then initial continuous maintenance infusion at 28 units/kg/hour.
- Adjust the drug to maintain an anti-Xa activity of 0.35 to 0.7 units/mL or an aPTT range that correlates to this anti-Xa range or a protamine titration range of 0.2 to 0.4 units/mL.
-
Children and Adolescents:
- In IV the Initial loading dose is 75 units/kg over 10 minutes, then initial continuous maintenance infusion at 20 units/kg/hour.
- Adjust heparin to maintain an anti-Xa activity of 0.35 to 0.7 units/mL or an aPTT range that correlates to this anti-Xa range or a protamine titration range of 0.2 to 0.4 units/mL.
-
It is noteworthy that because of variation among hospitals with reagents and corresponding control of aPTT values, individual institutions should establish unique, institution-specific nomograms based on the current reagents. Due to extensive variability within reagents and anti-Xa levels with corresponding aPTTs, a specific nomogram has not been provided and the physician should consult the local norms and guidelines.
-
Systemic to pulmonary artery shunt thrombosis (eg, Sano shunt, Blalock-Taussig shunt, central shunt); treatment in CHD patients:
-
Infants, Children, and Adolescents:
- It can be given as IV, 50 to 100 units/kg, an ongoing continuous infusion should be considered.
-
Pregnancy Risk Factor C
- Adverse effects were seen in animal studies. However, heparin does not cross the placenta.
- LMWH is used in thrombo-prophylaxis in pregnancy over unfractionated heparin.
- Twice day heparin should be stopped prior to induction of labor or a planned cesarean delivery.
- In pregnant women with mechanical heart valves, adjusted-dose LMWH or adjusted-dose heparin can be used throughout pregnancy or until week 13 of gestation when therapy can be changed to warfarin. LMWH or heparin should be resumed close to delivery.
- Warfarin can be used throughout pregnancy and replaced with LMWH or heparin near term. the use of low-dose aspirin is also recommended, in women who are at very high risk for thromboembolism having older generation prosthesis in mitral position or history of thromboembolism.
- When choosing therapy, fetal outcomes (ie, pregnancy loss, malformations), maternal outcomes (ie, VTE, hemorrhage), the burden of therapy, and maternal preference should be considered.
- Benzyl alcohol is contraindicated in pregnancy. Some products contain benzyl alcohol as a preservative.
Heparin use during breastfeeding:
- Heparin is not known to be secreted in breast milk.
- Some products contain benzyl alcohol as a preservative and their use in breastfeeding women is contraindicated by some manufacturers due to the association of gasping syndrome in premature infants.
Heparin Dose in Kidney Disease:
- No dosage adjustment required in patients with renal disease.
- Adjust therapeutic heparin according to aPTT or anti-Xa activity
Heparin Dose in Liver disease:
- No dose adjustment in liver diseases.
- Adjust therapeutic heparin according to aPTT or anti-Xa activity
Side effects of Heparin:
Thrombocytopenia can be seen between 0% and 30%. It is an immunologically mediated heparin-induced thrombocytopenia (HIT) that has been estimated to occur in 1% to 2% of patients and is marked by a progressive fall in platelet counts and, in some cases, thromboembolic complications like skin necrosis, pulmonary embolism, gangrene of the extremities, cerebrovascular accident, or myocardial infarction.
-
Cardiovascular:
- Chest Pain
- Shock (Including Hemorrhagic Shock)
- Thrombosis
- Vasospasm (Allergic; Possibly Related To Thrombosis)
-
Central Nervous System:
- Chills
- Dysesthesia (Feet)
- Headache
- Peripheral Neuropathy
-
Dermatologic:
- Dermal Ulcer (Rarely Reported With Deep Subcutaneous Injections; Intramuscular Injection [Not Recommended] Is Associated With A Higher Incidence Of This Effect)
- Eczema
- Erythematous Plaques (Case Reports)
- Localized Erythema (Rarely Reported With Deep Subcutaneous Injections; Intramuscular Injection [Not Recommended] Is Associated With A Higher Incidence Of This Effect)
- Skin Necrosis
- Transient Alopecia (Delayed)
- Urticaria
-
Endocrine & Metabolic:
- Adrenal Hemorrhage
- Hyperkalemia (Suppression Of Aldosterone Synthesis)
- Hyperlipidemia (Rebound; On Discontinuation)
- Ovarian Hemorrhage
-
Gastrointestinal:
- Constipation
- Hematemesis
- Melena
- Nausea
- Vomiting
-
Genitourinary:
- Erectile Dysfunction (Frequent Or Persistent Erection)
- Hematuria
-
Hematologic & Oncologic:
- Bruise (Unexplained)
- Gingival Hemorrhage
- Hematoma (Rarely Reported With Deep Subcutaneous Injections; Intramuscular Injection [Not Recommended] Is Associated With A Higher Incidence Of This Effect)
- Hemorrhage
- Pulmonary Hemorrhage
- Purpura
- Retroperitoneal Hemorrhage
- Thrombocytopenia (See Note)
-
Hepatic:
- Increased Liver Enzymes
-
Hypersensitivity:
- Anaphylactoid Reaction
- Hypersensitivity Reaction
-
Local:
- Local Irritation
- Local Pain (Rarely Reported With Deep Subcutaneous Injections; Intramuscular Injection [Not Recommended] Is Associated With A High Incidence Of These Effects)
-
Neuromuscular & Skeletal:
- Osteoporosis (Chronic Therapy Effect)
-
Ophthalmic:
- Allergic Conjunctivitis
- Lacrimation
-
Respiratory:
- Asthma
- Bronchospasm (Case Reports)
- Epistaxis
- Hemoptysis
- Rhinitis
-
Miscellaneous:
- Drug Tolerance
- Fever
Contraindications to Heparin:
- Hypersensitivity to heparin and any component of the formulation are contraindications.
- If severe thrombocytopenia is present. Previous history of heparin-induced hemoglobin (HIT)
- Other than when disseminated intravascular coagulation is involved, uncontrolled active bleeding can occur.
- Clinically harmful cases where sodium or chloride administration is required (large volume heparin 2 units/mL IV solutions only).
- It should not be used if appropriate blood coagulation tests are not available at the appropriate times (applicable to full-dose Heparin only).
Notice:Some products may contain benzyl alcohol, which is a preservative. It is not recommended that they be used in infants, neonates, pregnant, or breast-feeding women.
Warnings and precautions
-
Bleeding
- It can lead to fatal bleeding
- Patients at increased risk of bleeding (including subacute bacterial hemorhagic endocarditis) should be cautious. c
- Congenital and acquired bleeding disorders
- Active ulcerative or angiodysplastic GI disorders. Continuous GI tube drainage.
- Gravely uncontrolled hypertension, history hemorhagic stroke, and its use soon after brain, spine, or ophthalmologic surgeries or other invasive procedures such as spinal tap or spinal anesthesia, can lead to fatal complications.
- It is important to evaluate the effects of concurrent treatment with platelet inhibitors.
- Patients who have an antithrombin deficiency may experience unwanted side effects from concurrent antithrombin therapy.
- Grave liver disease
- Patients (especially women) over 60 years old may have hypertensive, diabetic, or diabetic retinopathy.
- Watch out for bleeding symptoms or signs in patients.
- If bleeding occurs, discontinue use. Protamine may be required for severe hemorhage or excessive dosing. Consult the Protamine monograph to learn more.
-
Heparin resistance:
- Patients with antithrombin deficiencies may require a dose of >35,000 units/24 hrs to maintain therapeutic aPTT.
- This could lead to an increase in heparin clearance, increased levels in heparin binding proteins, and elevations in factor VIII or fibrinogen.
- Patients with fever, thrombosis and thrombophlebitis, infections that have thrombosing tendencies, MI, or cancer are often affected by this resistance.
- It may be beneficial to measure anticoagulant effects by measuring anti-factorXa levels.
-
Hyperkalemia:
- Check for elevated potassium levels. This can lead to hyperkalemia and suppress aldosterone levels.
-
Hypersensitivity reactions
- Heparin should not be administered to patients who have a history of hypersensitivity reactions.
- Patients with allergies to animals (e.g. pork) may find some products that are made from animal tissue contraindicated. It is important to follow local guidelines.
-
Osteoporosis
- This can happen if you are using your device for longer than six months.
-
Thrombocytopenia:
- Heparin-induced hemocytopenia (HIT), a serious antibody-mediated reaction that results from irreversible platelet aggregation, can occur.
- Patients with HIT may develop a new thrombus.
- Pay attention to platelets. If platelets fall below 100,000/mm3 or thrombosis occurs, discontinue therapy.
- HIT and HITT can be delayed, and may occur several weeks after stopping heparin.
- Avoid patients who have had a history of HIT.
Heparin (unfractionated): Drug Interaction
|
Risk Factor C (Monitor therapy) |
|
|
5-Aminosalicylic Acid Derivatives |
May enhance the adverse/toxic effect of Heparin. Specifically, the risk for bleeding/bruising may be increased. |
|
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.) |
May enhance the anticoagulant effect of Anticoagulants. |
|
Aliskiren |
Heparin may enhance the hyperkalemic effect of Aliskiren. |
|
Angiotensin II Receptor Blockers |
Heparin may enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. |
|
Angiotensin-Converting Enzyme Inhibitors |
Heparin may enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. |
|
Antithrombin |
May enhance the anticoagulant effect of Heparin. |
|
Aspirin |
May enhance the anticoagulant effect of Heparin. |
|
Bromperidol |
May enhance the adverse/toxic effect of Anticoagulants. |
|
Caplacizumab |
May enhance the anticoagulant effect of Anticoagulants. |
|
Collagenase (Systemic) |
Anticoagulants may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. |
|
Corticorelin |
Heparin may enhance the adverse/toxic effect of Corticorelin. Significant hypotension and bradycardia have been previously attributed to this combination. |
|
Dasatinib |
May enhance the anticoagulant effect of Anticoagulants. |
|
Deferasirox |
Anticoagulants may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. |
|
Deoxycholic Acid |
Anticoagulants may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. |
|
Eplerenone |
Heparin may enhance the hyperkalemic effect of Eplerenone. |
|
Factor X (Human) |
Anticoagulants (Inhibitors of Factor Xa) may diminish the therapeutic effect of Factor X (Human). |
|
Fat Emulsion (Fish Oil Based) |
May enhance the anticoagulant effect of Anticoagulants. |
|
Ibritumomab Tiuxetan |
Anticoagulants may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to an increased risk of bleeding. |
|
Ibrutinib |
May enhance the adverse/toxic effect of Anticoagulants. |
|
Inotersen |
May enhance the anticoagulant effect of Anticoagulants. |
|
Limaprost |
May enhance the adverse/toxic effect of Anticoagulants. The risk for bleeding may be increased. |
|
Nintedanib |
Anticoagulants may enhance the adverse/toxic effect of Nintedanib. Specifically, the risk for bleeding may be increased. |
|
Nitroglycerin |
May diminish the anticoagulant effect of Heparin. Nitroglycerin may decrease the serum concentration of Heparin. |
|
Nonsteroidal Anti-Inflammatory Agents |
May enhance the anticoagulant effect of Anticoagulants. |
|
Obinutuzumab |
Anticoagulants may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. |
|
Omega-3 Fatty Acids |
May enhance the anticoagulant effect of Anticoagulants. |
|
Palifermin |
Heparin may increase the serum concentration of Palifermin. Management: If heparin is used to maintain an intravenous line, rinse the line with saline prior to and after palifermin administration. |
|
Pentosan Polysulfate Sodium |
May enhance the anticoagulant effect of Anticoagulants. |
|
Pentoxifylline |
May enhance the anticoagulant effect of Heparin. |
|
Potassium Salts |
Heparin may enhance the hyperkalemic effect of Potassium Salts. |
|
Potassium-Sparing Diuretics |
Heparin may enhance the hyperkalemic effect of PotassiumSparing Diuretics. Management: Monitor serum potassium concentrations closely. The spironolactone Canadian product monograph lists its combination with heparin or low molecular weight heparins as contraindicated. |
|
Prostacyclin Analogues |
May enhance the adverse/toxic effect of Anticoagulants. Specifically, the antiplatelet effects of these agents may lead to an increased risk of bleeding with the combination. |
|
Salicylates |
May enhance the anticoagulant effect of Anticoagulants. |
|
Sugammadex |
May enhance the anticoagulant effect of Anticoagulants. |
|
Sulodexide |
May enhance the anticoagulant effect of Anticoagulants. |
|
Thrombolytic Agents |
May enhance the anticoagulant effect of Anticoagulants. Management: See full drug monograph for guidelines for the use of alteplase for acute ischemic stroke during treatment with oral anticoagulants. |
|
Tibolone |
May enhance the anticoagulant effect of Anticoagulants. |
|
Tipranavir |
May enhance the anticoagulant effect of Anticoagulants. |
|
Tobacco (Smoked) |
May decrease the serum concentration of Heparin. |
|
Vitamin E (Systemic) |
May enhance the anticoagulant effect of Anticoagulants. |
|
Vitamin K Antagonists (eg, warfarin) |
Anticoagulants may enhance the anticoagulant effect of Vitamin K Antagonists. |
|
Risk Factor D (Consider therapy modification) |
|
|
Desirudin |
Anticoagulants may enhance the anticoagulant effect of Desirudin. |
|
Estrogen Derivatives |
May diminish the anticoagulant effect of Anticoagulants. More specifically, the potential prothrombotic effects of some estrogens and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of estrogens against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. Exceptions: Tibolone. |
|
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry) |
May enhance the adverse/toxic effect of Anticoagulants. Bleeding may occur. |
|
Progestins |
May diminish the therapeutic effect of Anticoagulants. More specifically, the potential prothrombotic effects of some progestins and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of progestins against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. |
|
Risk Factor X (Avoid combination) |
|
|
Apixaban |
May enhance the anticoagulant effect of Anticoagulants. Refer to separate drug interaction content and to full drug monograph content regarding use of apixaban with vitamin K antagonists (eg, warfarin, acenocoumarol) during anticoagulant transition and bridging periods. |
|
Dabigatran Etexilate |
May enhance the anticoagulant effect of Anticoagulants. Refer to separate drug interaction content and to full drug monograph content regarding use of dabigatran etexilate with vitamin K antagonists (eg, warfarin, acenocoumarol) during anticoagulant transition and bridging periods. |
|
Edoxaban |
May enhance the anticoagulant effect of Anticoagulants. Refer to separate drug interaction content and to full drug monograph content regarding use of edoxaban with vitamin K antagonists (eg, warfarin, acenocoumarol) during anticoagulant transition and bridging periods. Management: Some limited combined use may be indicated during periods of transition from one anticoagulant to another. See the full edoxaban drug monograph for specific recommendations on switching anticoagulant treatment. |
|
Hemin |
May enhance the anticoagulant effect of Anticoagulants. |
|
MiFEPRIStone |
May enhance the adverse/toxic effect of Anticoagulants. Specifically, the risk of bleeding may be increased. |
|
Omacetaxine |
Anticoagulants may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of anticoagulants with omacetaxine in patients with a platelet count of less than 50,000/uL. |
|
Oritavancin |
May diminish the therapeutic effect of Heparin. Specifically, oritavancin may artificially increase the results of laboratory tests commonly used to monitor IV heparin effectiveness, which could lead to incorrect decisions to decrease heparin doses. |
|
Rivaroxaban |
Anticoagulants may enhance the anticoagulant effect of Rivaroxaban. Refer to separate drug interaction content and to full drug monograph content regarding use of rivaroxaban with vitamin K antagonists (eg, warfarin, acenocoumarol) during anticoagulant transition and bridging periods. |
|
Streptokinase |
May enhance the anticoagulant effect of Heparin. |
|
Telavancin |
May diminish the therapeutic effect of Heparin. Specifically, telavancin may artificially increase the results of laboratory tests commonly used to monitor IV heparin effectiveness, which could lead to incorrect decisions to decrease heparin doses. |
|
Urokinase |
May enhance the anticoagulant effect of Anticoagulants. |
|
Vorapaxar |
May enhance the adverse/toxic effect of Anticoagulants. More specifically, this combination is expected to increase the risk of bleeding. |
Monitoring parameters:
- Hemoglobin and hematocrit.
- signs of bleeding including a fecal occult blood test.
- aPTT (or anti-factor Xa activity levels) or ACT depending upon indication.
- Platelet counts should be routinely monitored (eg, every 2 to 3 days on days 4 to 14 of heparin therapy) when the risk of HIT is more than 1% (eg, receiving therapeutic dose heparin, postoperative antithrombotic prophylaxis).
- If the patient has received heparin or low molecular weight heparin (eg, enoxaparin) within the past 100 days, if pre-exposure history is uncertain, or if an anaphylactoid reaction to heparin occurs then the chance of HIT is more common.
- When the risk of HIT is less than 1% (eg, medical/obstetrical patients receiving heparin flushes), routine platelet count monitoring is not recommended.
- For intermittent IV injections, aPTT is measured 3.5 to 4 hours after IV injection.
- It is noteworthy that continuous IV infusion is preferred over IV intermittent injections.
- For full-dose heparin (ie, non-low-dose), the dose should be titrated to an aPTT prolongation that corresponds to plasma heparin levels of 0.3 to 0.7 units/mL of the anti-Xa activity or 0.2 to 0.4 unit/mL by protamine titration.
- Because of variation among hospitals in the control aPTT values, nomograms should be established at each institution, designed to achieve aPTT values in the target range.
- Measurements should be made prior to heparin therapy, 6 hours (and in pediatric age group: 4 hours) after initiation, and 6 hours (pediatric: 4 hours) after any dosage change, and should be used to adjust the heparin infusion until the aPTT exhibits a therapeutic level.
- When two consecutive aPTT values are therapeutic, subsequent measurements may be made every 24 hours, and if necessary, dose adjustment carried out.
- In addition, a significant change in the patient's clinical condition (eg, recurrent ischemia, bleeding, hypotension) should prompt an immediate aPTT determination, followed by dose adjustment if necessary. In general, may increase or decrease infusion by 2 to 4 units/kg/hour dependent upon aPTT.
How to administer Heparin?
SubQ:
- Inject in subcutaneous tissue only (not muscle tissue).
- Injection sites should be rotated (usually left and right portions of the abdomen, above iliac crest).
IM administration:
- Do not administer IM due to pain, irritation, and hematoma formation.
Continuous IV infusion:
- Infuse via an infusion pump. If preparing a solution, mix thoroughly prior to administration.
Heparin lock:
- Inject via injection cap using positive pressure flushing technique.
- Heparin lock flush solution is intended only to maintain the patency of IV devices and is not to be used for anticoagulant therapy.
- Central venous catheters:
- Must be flushed with heparin solution when newly inserted, daily (at the time of tubing change), after blood withdrawal or transfusion, and after an intermittent infusion through an injectable cap.
- A volume of at least 10 mL of blood should be removed and discarded from a heparinized line before blood samples are sent for coagulation testing.
- Intravesical (off-label use):
- Various dosage regimens of heparin (20,000 to 50,000 units) alone or with alkalinized lidocaine (1% to 4%) have been instilled into the bladder.
Mechanism of action of Heparin:
- It activates antithrombin III, which inactivates thrombin and other coagulation factors IXa and Xa.
- Heparin stimulates also the release of lipoprotein Lipase (lipoprotein lipse hydrolyzes triglycerides to glycolic acid and free fatty acids).
Notice:
- There is a greater interpatient variability in pharmacokinetic parameters for pediatric patients than in adults.
- However, there have been reports of age-related decreases of volume distribution and clearance as a result of increasing pediatric patient age.
The onset of action: Anticoagulation:
- IV: Immediate;
- SubQ: ~20 to 30 minutes
Absorption:
- Oral, rectal: Erratic at best from these routes of administration;
- SubQ absorption is also erratic but considered acceptable for prophylactic use.
Metabolism:
- Complex; It is thought to occur by depolymerization and desulphation via the reticuloendothelial system primarily in the liver and spleen.
Half-life elimination:
- Age-related:
- Shorter half-life reported in premature neonates compared to adult patients
- Premature neonates GA 25 to 36 weeks (data based on a single dose of 100 units/kg within 4 hours of birth): Mean range: 35.5 to 41.6 minutes.
- Dose-dependent:
- IV bolus: 25 units/kg: 30 minutes.
- If 100 units/kg: then should be given over 60 minutes.
- If 400 units/kg: then it should be given over 150 minutes.
- Mean: 1.5 hours.
- Range: 1 to 2 hours.
- Its half-life is affected by obesity, renal function, malignancy, presence of pulmonary embolism, and infections.
Note:
- At therapeutic doses, elimination occurs rapidly via nonrenal mechanisms.
- With very high doses, renal elimination may play more of a role; however, dosage adjustment remains unnecessary for patients with renal impairment.
Excretion:
- Urine (small amounts as unchanged drug);
- Note:
- At therapeutic doses, elimination occurs rapidly via nonrenal mechanisms.
- With very high doses, renal elimination may play more of a role.
- However, dosage adjustment remains unnecessary for patients with renal impairment.
Clearance:
- Clearance is different at different ages.
- Within a neonatal population, slower clearance with lower GA. However, when compared to adults, the overall clearance in neonatal and pediatric patients is faster than adults.
International Brand Names of Heparin:
- Heparin Leo
- Agglutek
- Anticlot
- Caprin
- Coaparin
- Haidyparin
- Hemastat
- Hemonor
- Hepaflex
- Heparen
- Heparil
- Heparin
- Heparin Injection B.P.
- Heparin Leo
- Heparin Novo
- Heparin Sodium B Braun
- Heparina
- Heparine
- Heparine Choay
- Heparine Novo
- Heprin
- Hepsal
- Heptin
- Inhepar
- Inviclot
- Kabihep
- Lioton
- Liquemin
- Liquemine
- Lyogel
- Minihep
- Monoparin
- Multiparin
- Nuparin
- Pharepa
- Proparin
- Rhoneparina
- Sakarin
- Thrombophob
- Thrombophob-S
- Thromboreduct
- Unihep
- Wellparin
Heparin Brand Names in Pakistan:
- Heparin Sodium Injection 5000 IU/ml (Total: 25000 IU/ 5ml): B-Braun