Sitaphage is a diabetes pill containing Sitagliptin and metformin. Sitaphage brand is marketed by Martin Dow, manufacturer of the original Glucophage (metformin). Sitaphage possesses some of the properties of ideal diabetes medicine.
These will be discussed one by one here. Diabetes is a global disease, a pandemic nowadays. There are over 463 million people worldwide with diabetes and 1.6 million of them die each year.
As of today (09th June 2021), the total number of COVID cases worldwide has been around 174 million, and 3.75 million people have died of COVID-19 infection [Ref]. In a survey conducted in Pakistan in 2016-2017 [Ref], it was estimated that one out of every fourth adult in Pakistan is diabetic (the overall prevalence was 26.3%). 14.47% of the adult population had diabetes.
Thus, about 40% of Pakistani adults are either diabetics or have prediabetes. Comorbid conditions were as follows:
- Hypertension: 46.2%
- Hypercholesterolemia: 39.3%
- Obesity: 43.9%
The total number of diabetic patients was estimated in 2019 to be around 463 million. The numbers are expected to reach 700 million in 2045 (with an average increase of 51%). The greatest increase in the percentage of diabetics is expected in the Asian, African, and Middle Eastern regions - affecting mostly the low-income countries.
How does diabetes progress over time?
Diabetes rarely develops acutely as may occur in patients with pancreatitis, viral infections, and steroids intake. The pathophysiologic mechanisms usually start years before the diagnosis is made. These abnormalities include:
- Beta-cell loss and dysfunction,
- Insulin resistance and
- Altered insulin secretion.
It has been estimated that at the onset of diabetes, only 50% of the beta cells are left. Beta-cell loss starts around 10 years before the diagnosis of Diabetes along with insulin resistance. Initially, the rise in blood sugars is compensated by a rise in insulin levels.
The diagnosis is made an average of five years after the onset of diabetes. The microvascular and macrovascular complications have already developed when the diagnosis of diabetes is made.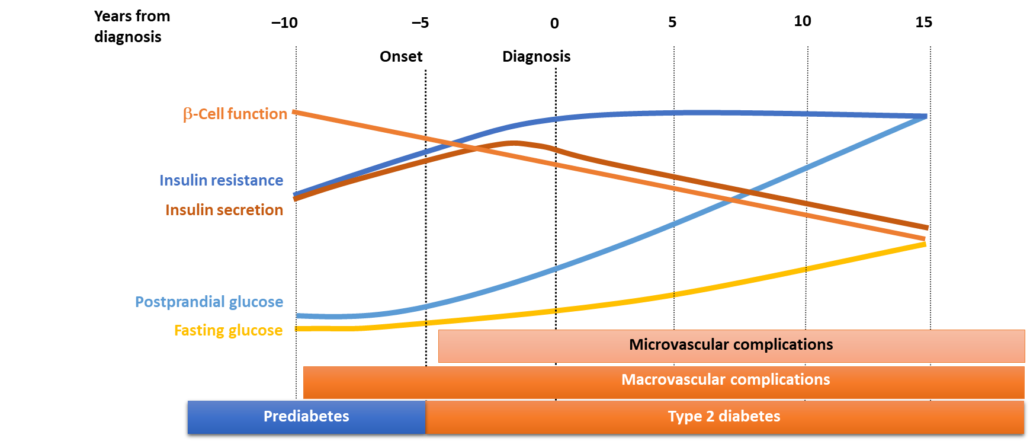
Beta-cell dysfunction starts as early as ten years before the diagnosis of diabetes is made. Most patients at this time have already developed diabetes-related complications
To understand the role of SITAPHAGE in the management of Diabetes, it is important to understand the basic mechanisms that result in hyperglycemia. Diabetes develops as a result of:
- Insulin resistance,
- Insulin secretory defects, and
- Increased hepatic output.
What causes these defects is not fully understood. However, the incretin effect is now well understood. Incretins are hormones released in response to oral glucose.
The body senses the glucose stimuli before even it is ingested by the person. In response to a glucose load, the body releases the hormones called incretins. The word INCRETIN has been derived from "INtestinal seCRETion of INsulin". There are two main incretins:
- GIP (originally “gastric inhibitory polypeptide,” later renamed “glucose-dependent insulinotropic polypeptide”) and
- GLP-1 (glucagon-like peptide 1)
What is the Incretin effect:
The incretin effect was demonstrated initially when a greater rise in plasma insulin was noted with oral glucose compared to intravenous glucose. The incretin effect is demonstrated here: 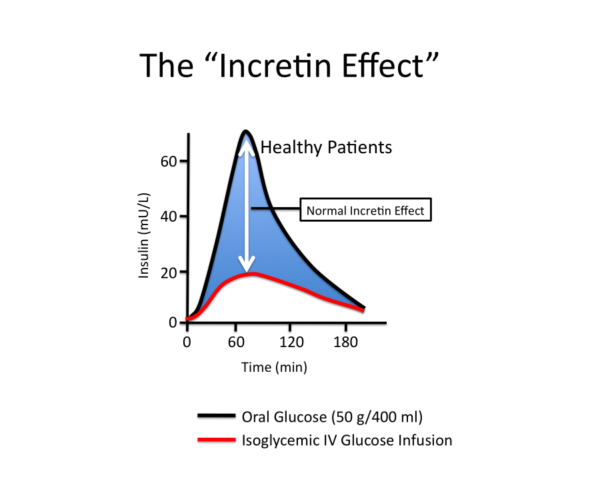
Compared to intravenous glucose, there is a significant increase in insulin secretion when glucose is administered orally.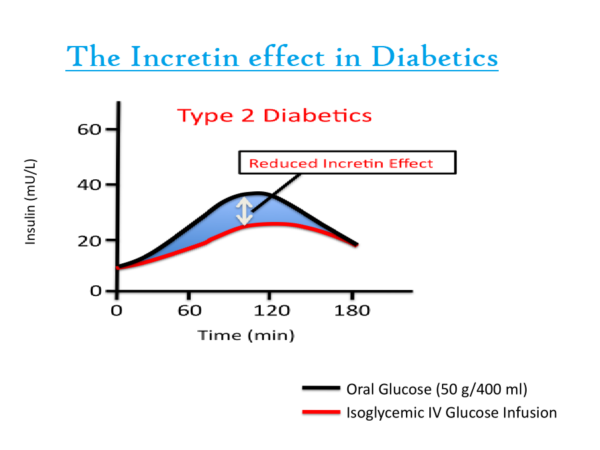
The incretin effect in diabetics is blunted compared to healthy individuals. If you give intravenous glucose, the plasma insulin rise, however, if you give a person oral glucose, there is a significant rise in the plasma glucose levels.
This difference is due to the incretin effect. The rise in insulin is blunted in patients with diabetes compared to normal subjects.
How do DPP-IV inhibitors (Sitagliptin) act (Mechanism of action of Sitagliptin)?
Sitagliptin inhibits the enzyme DPP-IV. This enzyme is responsible for the degradation of endogenous incretins. As the enzyme is inhibited, the plasma levels of incretins increase and they stay in the plasma for a longer time than usual. Thus sitagliptin indirectly reduces blood glucose by stimulating insulin release and suppressing glucagon in a glucose-dependent mechanism.
How does Sitaphage target the "Triad Core" Defects of Diabetes?
Since Sitaphage is a combination of Sitagliptin and Metformin, it exerts its effects through the combined roles of sitagliptin and metformin. Sitagliptin increases insulin synthesis and secretion by improving beta-cell function.
It also preserves beta-cell mass and hence has a protective role. It also suppresses hepatic glucose output by inhibiting the release of glucagon. Metformin, on the other hand, reduces insulin resistance in the peripheral cells.
It also reduces the hepatic glucose output by inhibiting gluconeogenesis and glycogenolysis. The triad is well demonstrated here: 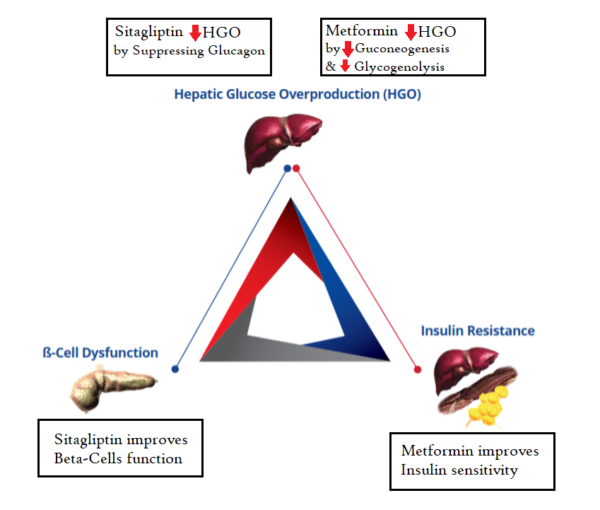 Sitaphage (Sitagliptin and metformin) targets the triad core defects of Diabetes
Sitaphage (Sitagliptin and metformin) targets the triad core defects of Diabetes
How to manage diabetes with oral drugs:
Diabetes management should be focused on. It should not be aimed to reduce blood sugar levels only. It should include lifestyle modifications such as a healthy diabetic and cardiovascular diet, smoking cessation, and management of comorbid conditions like high blood pressure, dyslipidemias, and antiplatelets. 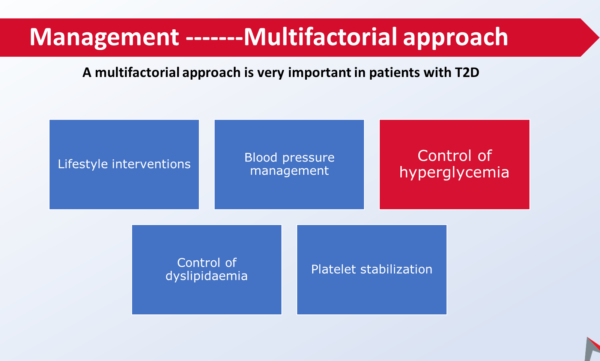 Diabetes management should be focused and multifactorial.
Diabetes management should be focused and multifactorial.
However, glycemic control is our primary concern. Here, this illustration shows us what happens when your glycated hemoglobin improves by a 1 percentage point. 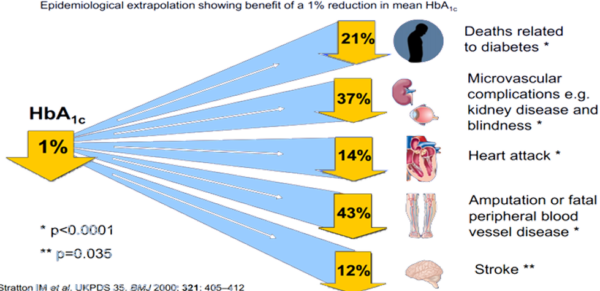 1% reduction in the glycated hemoglobin results in a marked improvement in all diabetes-related complications
1% reduction in the glycated hemoglobin results in a marked improvement in all diabetes-related complications
Diabetes-related mortality declines by 21%, microvascular complications such as nephropathy and retinopathy by 37%, the risk of Myocardial infarction is reduced by 14%, Peripheral arterial disease and the risk of amputations decline by 43%, the stroke risks decline by 12%.
Benefits and Drawbacks of Metformin:
It is usually considered a first-line of medicine, although, recent guidelines now suggest individualizing the treatment as per the patient comorbid conditions and tolerance.
- Efficacy:
- Metformin is effective in most patients and reduces the HbA1C by 1 – 2%.
- Hypoglycemia and its effect on weight:
- It rarely causes hypoglycemia and may induce slight weight loss.
- Renal and genitourinary effects:
- It is not indicated in advanced kidney disease when the CrCl falls to 30 ml/minute or less.
- GI side effects:
- It may not be tolerated by some patients because of the GIT side effects especially when given in high doses. Some of the patients may tolerate the modified release formulations.
- Cardiac effects:
- It has some cardioprotective and antioxidant properties and is recommended as the first line of treatment in diabetic patients with stable heart failure.
- Bones and Ketoacidosis:
- It does not have any effect on the bones and does not cause ketoacidosis.
Advantages and disadvantages of DPP IV inhibitors:
These drugs include sitagliptin vildagliptin, linagliptin, and saxagliptin
- Efficacy in Diabetes:
- These drugs are moderately effective in reducing glycated hemoglobin.
- Hypoglycemia and weight loss:
- These drugs do not cause hypoglycemia and are weight neutral.
- Effect on kidneys and genitourinary effects:
- They are effective in reducing albuminuria. In advanced kidney disease, dosage adjustment is required except for linagliptin which may be given without the need to adjust the dose.
- Cardiac effects:
- These drugs may be used in heart failure except for saxagliptin and alogliptin. It also reduces plasma lipid levels and may have some beneficial effects as well.
- Effect on bones and ketoacidosis:
- It does not cause ketoacidosis and has minimal effects on bones.
Advantages and Disadvantages of SGLT2 inhibitors:
SGLT2 inhibitors include dapagliflozin (Farxiga), empagliflozin (Jardiance), and ertugliflozin (Steglatro).
- Efficacy in Diabetes:
- These drugs are moderately effective like sitagliptin (or maybe less effective).
- Hypoglycemia and weight loss:
- These drugs do not cause hypoglycemia and induce weight loss.
- Renal and Genitourinary effects:
- These drugs have diuretic-like properties and may cause dehydration resulting in acute renal failure.
- UTIs and genital infections are the most common complications associated with these drugs, particularly in females.
- In stable patients with diabetic nephropathy, these drugs may stop the progression of CKD.
- GI side effects:
- They do not have GIT side effects.
- Cardiac effects:
- Diabetic patients with heart failure benefit the most from SGLT2 inhibitors.
- Effect on bones and ketoacidosis:
- These drugs may increase the risk of amputations and fractures and cause euglycemic ketoacidosis.
- Most experts recommend avoiding SGLT2 inhibitors in diabetic patients with covid 19 infections as the risk of euglycemic ketoacidosis is increased.
Insulin secretagogues:
These drugs primarily include sulfonylureas and meglitinides (repaglinide and nateglinide).
- Efficacy:
- These drugs are highly effective
- Effect on weight and hypoglycemia:
- There is a moderate to severe risk of hypoglycemia. It also causes weight gain.
- Renal and genitourinary effects:
- These drugs can increase the risk of hypoglycemia in patients with impaired renal functions and should be avoided in advanced kidney disease. They do not have genitourinary adverse effects.
- GI side effects:
- They are better tolerated and do not have GI side effects.
- Cardiac effects:
- They may increase the risk of atherosclerotic cardiovascular diseases and heart failure and should be avoided in patients with cardiac diseases.
- Bones and ketoacidosis:
- They do not have any effects on bones and do not cause ketoacidosis.
Key points from clinical trials:
- Sitagliptin in combination with metformin (Sitaphage) is more effective in reducing the glycated hemoglobin compared to either drug alone [Ref].
- Compared to Glimepiride and metformin combination, Sitaphage (sitagliptin and metformin combination) is associated with a reduced risk of hypoglycemia [Ref].
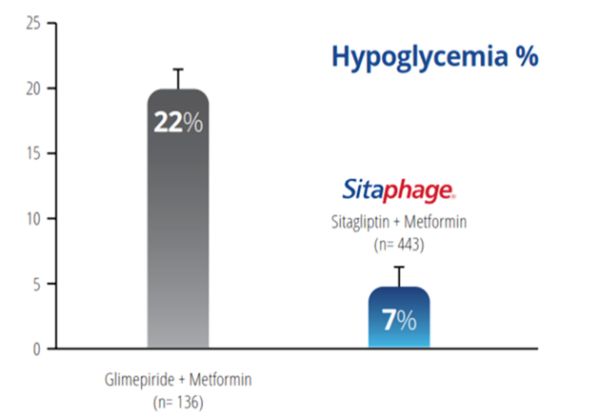 Sitaphage (sitagliptin and metformin) is associated with a lower risk of hypoglycemia compared to glimepiride and metformin.
Sitaphage (sitagliptin and metformin) is associated with a lower risk of hypoglycemia compared to glimepiride and metformin.
The symptoms of hypoglycemia may vary depending on the severity. Patients may develop confusion, and irritability, resulting in falls and accidents and may cause permanent neurological deficits.
Frequent hypoglycemia may also manifest as dementia later in life. Patients may not be aware of hypoglycemia if they have concomitant autonomic neuropathy or have recurrent hypoglycemia. Hypoglycemia may also result in cardiovascular events such as cardiac arrhythmias and angina.
-
The Cardiovascular safety of Sitaphage:
- CVS safety of antidiabetic medicines is an important parameter. Evaluating cardiac safety has been made compulsory for all drugs before they are approved. Cardiovascular diseases are more common in diabetics compared to non-diabetics, especially in the aged population.
- The Cardiovascular safety of Sitagliptin was proved in the TECOS trial. The results are tabulated here:
|
Clinical outcomes |
Risk Reduction by Sitagliptin |
|
Hospitalization for Unstable Angina |
10% |
|
Fatal & Non-Fatal MI |
5% |
|
Fatal and Non-Fatal Stroke |
3% |
|
Hospitalization for HF (Sita vs Placebo) |
Non-Inferior to Placebo/ Neutral |
- The Cardiovascular safety of metformin was proved in the UKPDS Trial. Here is the evidence in tabulated form:
|
Clinical outcomes |
Risk Reduction by Metformin |
|
Any Diabetes-related endpoint |
32% |
|
Diabetes-related Death |
42% |
|
All-cause mortality |
36% |
|
Microvascular disease |
29% |
|
Myocardial Infraction |
39% |
|
Fatal Myocardial Infraction |
50% |
|
Stroke |
41% |
How incretins improve the cardiovascular profile in diabetic patients:
- The primary effect is of course its effect on blood sugars without increasing the risk of hypoglycemia.
- It increases satiety and suppresses hunger resulting in weight loss.
- It reduces the risk of myocardial injury
- Improves dyslipidemia
- Reduces blood pressure
- And improves the endothelial function
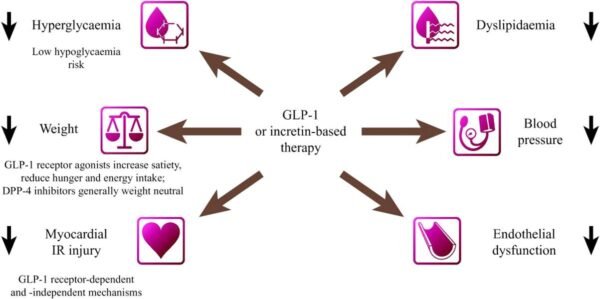 and how incretins-based therapies exert a beneficial effect on the heart and cardiovascular system.
and how incretins-based therapies exert a beneficial effect on the heart and cardiovascular system.
As DPP 4 inhibitors primarily act by increasing the levels of incretins, these effects can be partly attributed to DPP IV inhibitors as well.
-
Effect on Dyslipidemia compared to glimepiride:
- Sitaphage exerts a beneficial effect on dyslipidemia and has a pleiotropic effect in inhibiting cardiovascular disease compared to glimepiride.
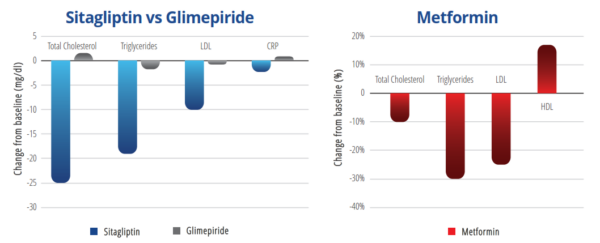
After 12 weeks of treatment, body weight increased in glimepiride but slightly reduced in sitagliptin, however, the comparison between them was non-significant (p=0.07). Although both groups reduced blood sugar and HbA1c, the comparison between them was non-significant (p=0.59 and p=0.17 respectively). Lipid profile improved significantly in sitagliptin vs. glimepiride group as mentioned below:
- Total cholesterol (-25±32.5 vs +1.5±45.4 P=0.02)
- Triglycerides (-19±44.6 vs-1.8±48.7 P=0.001)
- LDL- cholesterol (-10±22.4 vs-0.8±18.7 P=0.001)
- HDL-cholesterol (-2.6±6.2 vs 1.2±5.2 P=0.03).
Sitagliptin significantly reduced CRP in comparison to glimepiride (-2.3±1.8 vs0.8±1.5 P=0.001).
Sitagliptin has a beneficial effect in patients with diabetic nephropathy:
CKD staging is done on the basis of estimated GFR and albuminuria. It is classified as A1, A2, and A3 based on albumin excretion in the urine. A1 is urinary albumin excretion of less than 30 mg, A2 is the stage of microalbuminuria or urinary albumin excretion of 30 to 300 mg/day, and A3 is albumin excretion of greater than 300 mg/day or the stage of macroalbuminuria. GFR basis classification is another way.
Clinically, a GFR of less than 60 ml/minute is labeled as CKD. As kidney function declines, the risk of death from a cardiovascular cause is significantly increased.
Microalbuminuria corresponds to early diabetic nephropathy, macroalbuminuria corresponds to progressive diabetic nephropathy. With sitagliptin, a significant reduction is seen in both parameters. Sitagliptin improves albuminuria without decreasing the GFR. 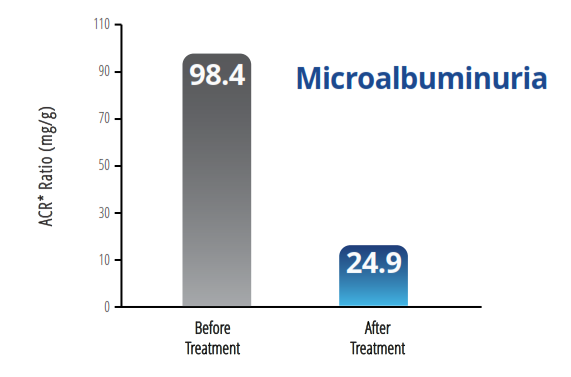 sitagliptin effect in patients with early diabetic nephropathy.
sitagliptin effect in patients with early diabetic nephropathy.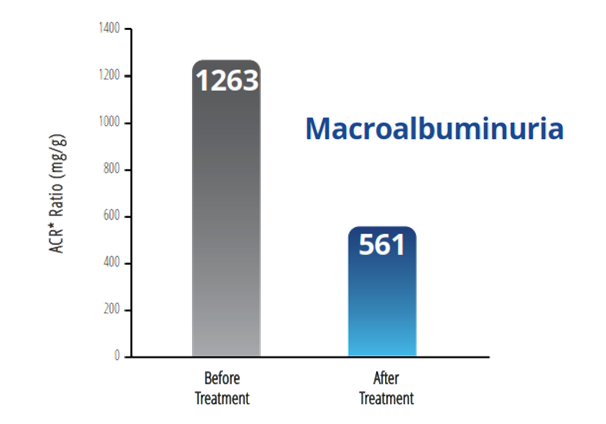 sitagliptin effect in patients with progressive diabetic nephropathy.
sitagliptin effect in patients with progressive diabetic nephropathy.
Add-on therapy to metformin, sitagliptin may provide greater reductions in albuminuria independent of glycemic control when compared to SU.
Sitagliptin improves albuminuria in patients with Type 2 Diabetes mellitus:
|
Sitagliptin |
Urine albumin (mg/g) |
Log (urine albumin) |
|
Baseline |
68.9 – 133.4 |
1.3 – 0.7 |
|
6 months |
42.2 – 126.4* |
1.0 – 0.6* |
|
% change |
-36.3 – 43.3† |
-23.3 – 37.9 † |
|
Other Glucose Lowering medicines |
||
|
Baseline |
61.4 – 154.3 |
1.2 – 0.6 |
|
6 months |
81.2 – 194.5 |
1.3 – 0.6 |
|
% change |
112.5 – 255.0 |
0.8 – 192.0 |
In Conclusion:
Sitaphage has the ability to:
- Maintain beta-cell mass and preserves Beta-cell function,
- Effectively controls blood glucose levels without increasing the incidence of hypoglycemia or weight gain,
- Improves cardio-renal function
- Reduces CV risk factors e.g. Lipid Profile
- In addition, combination therapy implements less than maximal doses of metformin permitting a minimum of metformin-associated gastrointestinal effects.
- The fixed-dose combination allows physicians to modify the regimens of patients with inadequately controlled glucose levels with metformin monotherapy without increasing the pill burden.
- Sitaphage is the combination of Original & Trusted Metformin with Sitagliptin in Fixed-Dose Combination.
- Sitaphage addresses Triad Core defect with Superior Glycemic Control
- It has an established Cardiovascular Safety profile
- Sitaphage is a safe, effective, and well-tolerated therapy in diabetic patients.







