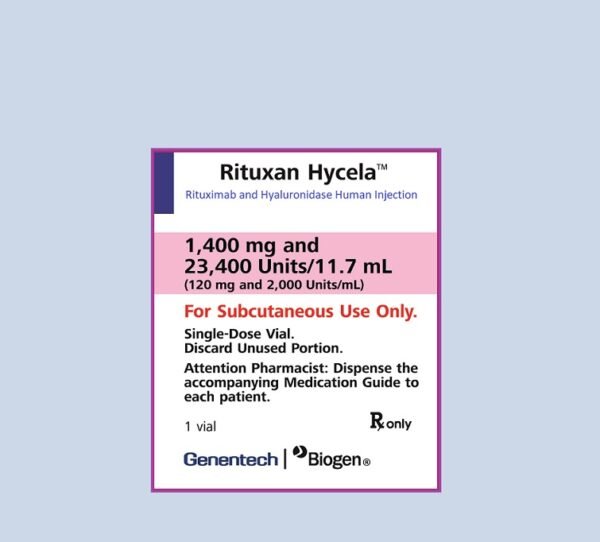
Rituximab and Hyaluronidase (Rituxan Hycela) is a combination of rituximab (that is a CD-20 directed IgG1 monoclonal antibody) and hyaluronidase (an enzyme that increases the permeability of subcutaneous tissue). It is used as a subQ injection in the treatment of chronic lymphocytic leukemia, diffuse large B-cell lymphoma, and follicular lymphoma.
Rituximab and Hyaluronidase (Rituxan Hycela) Uses:
Chronic lymphocytic leukemia:
- We can use this in adult patients along with fludarabine and cyclophosphamide to treat chronic lymphocytic leukemia either treated or untreated previously.
Diffuse large B-cell lymphoma:
- Can treat previously untreated diffuse large B-cell lymphoma (DLBCL) in combination with cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP) or other anthracycline-based chemotherapy regimens
Follicular lymphoma:
- It is used in adults to treat relapsed or refractory follicular lymphoma (FL) as a single agent;
- It is used to treat previously untreated follicular lymphoma(FL) (in combination with first-line chemotherapy) and, in patients achieving a complete or partial response to rituximab in combination with chemotherapy (as a single-agent )
- It is used to treat non-progressing (including stable disease) FL as a single agent after first-line cyclophosphamide, vincristine, and prednisone (CVP) chemotherapy
- Limitations of use:
- start rituximab/hyaluronidase only after patients have received at least 1 full dose of a rituximab product by intravenous(IV) infusion
- It is not indicated for non-malignant conditions.
Rituximab and Hyaluronidase (Rituxan Hycela) Dose in Adults
Note:
- Before initiation of therapy all patients must receive a test dose i.e at least one full intravenous rituximab dose without experiencing any reaction.
- patients who do not tolerate full IV dose should administer drug in subsequent cycles. May switch to subQ after success full administration of full IV dose.
- Premedicate with acetaminophen and an antihistamine before each dose (consider glucocorticoid premedication if necessary).
- For patients who have risk of tumor lysis syndrome consider anti- hyperuricemic therapy and aggressive hydration (high tumor burden or lymphocytes >25,000/mm³).
- In patients with chronic lymphocytic leukemia (CLL), Pneumocystis jirovecii pneumonia (PCP) and antiherpetic viral prophylaxis is recommended during treatment (and for up to 12 months following treatment).
Rituximab and Hyaluronidase (Rituxan Hycela) Dose in the treatment of Chronic lymphocytic leukemia:
- SubQ: Rituximab 1,600 mg/hyaluronidase 26,800 units (fixed dose) on day 1 of a 28-day cycle in cycles 2 through 6 (in combination with fludarabine and cyclophosphamide (IV rituximab should be administered in cycle 1).
Rituximab and Hyaluronidase (Rituxan Hycela) Dose in the treatment of Diffuse large B-cell lymphoma:
- SubQ: Rituximab 1,400 mg/hyaluronidase 23,400 units (fixed dose) on day 1 of cycles 2 through 8 in combination with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) (IV rituximab should be administered in cycle 1).
Rituximab and Hyaluronidase (Rituxan Hycela) Dose in the treatment of Follicular lymphoma:
Previously untreated:
- SubQ: Induction: Rituximab 1,400 mg/hyaluronidase 23,400 units (fixed dose) on day 1 of a 21-day cycle in cycles 2 through 8 (in combination with chemotherapy);
- IV rituximab should be administered in cycle 1.
- In patients with complete or partial response with combination chemotherapy, initiate maintenance treatment (see below).
Maintenance:
- SubQ: For patients with complete or partial response, initiate rituximab 1,400 mg/hyaluronidase 23,400 units (fixed dose) once every 8 weeks for 12 doses.
- Maintenance treatment should be initiated 8 weeks following completion of initial combination chemotherapy treatment.
Rituximab and Hyaluronidase (Rituxan Hycela) Dose in the treatment of Non-progressing disease following 6 to 8 cycles of first-line CVP chemotherapy:
- SubQ: Rituximab 1,400 mg/hyaluronidase 23,400 units (fixed dose) once per week for 3 weeks (IV rituximab should be administered in week 1 for a total of 4 weeks of therapy) at 6-month intervals to a maximum of 16 doses.
Relapsed or refractory:
- SubQ: Rituximab 1,400 mg/hyaluronidase 23,400 units (fixed dose) once weekly for 3 or 7 weeks (IV rituximab should be administered in week 1) for a total of 4 or 8 weeks of therapy
Relapsed or refractory (retreatment):
- SubQ: Rituximab 1,400 mg/hyaluronidase 23,400 units (fixed dose) once weekly for 3 weeks (IV rituximab should be administered in week 1) for a total of 4 weeks of therapy.
Rituximab and Hyaluronidase (Rituxan Hycela) Dose in Relapsed or refractory (maintenance treatment after response to induction treatment) [Canadian labeling]:
- SubQ: 1,400 mg (fixed-dose) once every 3 months until disease progression or maximum duration of 2 years (Rituxan SC Canadian product labeling)
Rituximab and Hyaluronidase (Rituxan Hycela) Use in Children:
This therapy for children is not recommended.
Pregnancy Risk Category: Not assigned
- Infants exposed to Rituximab in utero may experience adverse effects.
- Women of childbearing age should use contraceptives during treatment and for one-year afterward.
- For more information, refer to the individual monographs.
Use of Rituximab or hyaluronidase during lactation:
- It is unknown if breast milk contains rituximab and hyaluronidase.
- Human IgG is excreted from breast milk, so rituximab could be present.
- Breastfeeding mothers who are nursing should not continue to breastfeed during treatment or for more than 6 months after it is completed. For more information, refer to the individual monographs.
Dose in Kidney Disease:
No dosage adjustments are provided.
Dose in Liver disease:
No dosage adjustments are provided in the manufacturer’s labeling (has not been studied).
Also see individual agents. All incidences are from combination therapy regimens.
Common Side Effects of Rituximab and Hyaluronidase (Rituxan Hycela):
Central Nervous System:
- Fatigue
- Paresthesia
- Headache
- Peripheral Neuropathy
Dermatologic:
- Alopecia
- Allergic Skin Reaction
- Erythema
- Skin Rash
Gastrointestinal:
- Nausea
- Constipation
- Vomiting
- Diarrhea
- Abdominal Pain
Hematologic & Oncologic:
- Neutropenia
- Anemia
- Leukopenia
- Febrile Neutropenia
Immunologic:
- Antibody Development
Infection:
- Serious Infection
Local:
- Erythema At Injection Site
Neuromuscular & Skeletal:
- Weakness
- Arthralgia
Respiratory:
- Cough
- Upper Respiratory Tract Infection
- Dyspnea
- Pneumonia
Miscellaneous:
- Fever
Less Common Side Effects Of Rituximab and Hyaluronidase (Rituxan Hycela):
Cardiovascular:
- Peripheral Edema
- Chest Pain
- Hypertension
- Hypotension
Central Nervous System:
- Chills
- Insomnia
- Dizziness
Dermatologic:
- Pruritus
Endocrine & Metabolic:
- Weight Loss
Gastrointestinal:
- Decreased Appetite
- Dyspepsia
- Mucosal Inflammation
- Stomatitis
- Upper Abdominal Pain
Genitourinary:
- Urinary Tract Infection (UTI)
Hematologic & Oncologic:
- Lymphocytopenia
Infection:
- Influenza
Local:
- Pain At Injection Site
Neuromuscular & Skeletal:
- Limb Pain
- Ostealgia
- Back Pain
- Muscle Spasm
- Myalgia
Ophthalmic:
- Conjunctivitis
Respiratory:
- Nasopharyngitis
- Oropharyngeal Pain
- Bronchitis
- Sinusitis
- Flu-Like Symptoms
Frequency of Side effects not defined:
Hypersensitivity:
Allergic Reaction
Infection:
- JC Virus Infection
Local:
- Reaction at Site of Administration
Contraindications to Rituximab and Hyaluronidase (Rituxan Hycela):
The manufacturer's labeling does not list any contraindications. Canadian labeling
- Known type 1 hypersensitivity, anaphylactic reaction to murine proteins, Chinese Hamster Ovary cell proteins or any component of formulation
- Patients who have or had progressive multifocal encephalopathy (PML)
- Patients with active, severe infections.
Warnings and precautions
Perforation/obstructure of the Bowel
- Patients receiving rituximab have reported abdominal pain, intestinal obstruction and perforation (rarely fatal).
- The average onset time of symptoms is 6 days. (range: 1 - 77 days). Keep the patient in your care for any repeated vomiting or abdominal pain during treatment.
Cardiovascular effects
- Use of rituximab products may cause cardiovascular disorders (e.g., ventricular fibrillation and myocardial injury) during treatment.
- For serious or life-threatening arrhythmias, Rituximab/hyaluronidase should be discontinued.
- Assess the cardiac function of patients with arrhythmias, angina or a history of arrhythmia.
Cytopenias
- Rituximab can cause lymphopenia and leukopenia as well as neutropenia and thrombocytopenia. These cytopenias may last for months after treatment.
- Monitor CBC.
Hepatitis B virus activation: [US-Boxed Warning]
- Hepatitis B virus (HBV), reactivation can occur when rituximab is used in combination with rituximab/hyaluronidase.
- In some cases, this may lead to fulminant liver disease, hepatic failure and even death.
- Before starting treatment, screen all patients for HBV infection. Monitor patients throughout and after treatment.
- Stop taking rituximab/hyaluronidase or concomitant medication if there is HBV activation.
- Screening should include hepatitis B antigen (HBsAg), and hepatitis B key antibody (anti-HBc); patients should be monitored for signs and symptoms of hepatitis B or HBV reactivation, both clinically and lab.
- Antiviral therapy should be started in the event of viral hepatitis.
- Patients who have HBsAg elevated as well as those with anti-HBc antibodies but who have not been treated for the disease, may be reactivated.
- HBV reactivation can occur up to two years after rituximab is discontinued.
- Patients with evidence of HBV infection, such as HBsAg positive (regardless of antibody status) or HBsAg nil but anti-HBc positive (eg. HBsAg positive), should be treated cautiously. Consider appropriate antiviral treatment and monitoring prior to and/or during rituximab treatments.
- It is unknown if it is safe to resume rituximab-containing therapy after HBV activation. Talk to HBV specialists about reinitiation of therapy for patients with HBV reactivation.
- American Society of Clinical Oncology's provisional clinical opinion update regarding hepatitis B virus testing recommendations:
- AntiCD20 antibody-positive patients are at risk of hepatitis B virus reactivation.
- Before starting treatment, screen for HBV infection using HBsAg or anti-HBc tests. A total antiHBc test (with both IgG/IgM) or an anti-HBc IgG should be used. Anti-HBc IgM may not confirm acute HBV infections.
- Before initiating treatment, it is important to screen patients with risk factors for HBV infection, such as birthplace in a country with >=2% HBV incidence, sexual contact with HBV-infected persons, high-risk behavior [eg intravenous drug abuse] and HIV infection.
- For HBsAg/anti-HBc patients who are HBsAg positive/anti–HBc positive, start prophylactic antiviral treatment (using antivirals that have low viral resistance rates) and continue antivirals for 6 to 12 months.
- Patients with HBsAg 0/anti-HBc positive status should be tested for HBV reactivation by HBV DNA and ALT testing every 3 months. Antiviral therapy should be initiated promptly if there is any sign of HBV reactivation.
Hypersensitivity
- Allergy reactions to Rituximab may be due to cytokine release or other chemical mediators.
- Patients must be given at least one dose of intravenous Rituximab prior to administering subcutaneous Rituximab/hyaluronidase. This is because of the high risk of hypersensitivity.
- Most infusion-related reactions occur within 30 to 120 min and can include hypotension, bronchospasm and hypoxia. In more severe cases, pulmonary infiltrates and acute respiratory distress syndrome may also be present.
- Hypersensitivity and other reactions can occur, usually within minutes of infusion initiation. Severe cytokine release syndromes may develop within one to two hours.
- Patients with a history or pulmonary tumor infiltration are not likely to have a good prognosis.
- Patients with a history or preexisting conditions, or patients with a high number of malignant cells (>25,000/mm3) should be evaluated regularly.
- Premedicate patients with acetaminophen or an antihistamine before administering drugs.
- Subcutaneous injections should be observed for at least 15 minutes. Patients with high hypersensitivity may need to be watched longer.
- If you notice severe reactions, stop giving rituximab/hyaluronidase immediately and begin aggressive symptomatic management.
- In the event of an allergic reaction, you should immediately have access to bronchodilators and epinephrine as well as antihistamines and corticosteroids.
Infections
- After or during therapy, serious and potentially fatal fungal, bacterial and viral infections can occur.
- Patients with hypogammaglobulinemia (hypogammaglobulinemia that persists for more than 11 months) have had infections.
- There may be hepatitis B or C, varicella-zoster, West Nile virus, parvovirus B19 and herpes simplex viruses such as cytomegalovirus and parvovirus B19.
- If you have serious infections, stop using it and get the appropriate treatment.
[US Boxed Warning]: Mucocutaneous and cutaneous reactions
- Patients who receive rituximab/hyaluronidase and products containing it may experience severe, even fatal, mucocutaneous reaction.
- Reports of paraneoplastic pemphigus and Stevens-Johnson Syndrome, Stevens – Johnson syndrome, lichenoid, vesiculobullous, and toxic epidermal necrolysis have been made.
- Patients with severe skin reactions should discontinue use. The safety of reexposure for patients suffering from mucocutaneous reactions is not known.
- Subcutaneous rituximab may cause localized cutaneous reactions (eg, pain and swelling at the injection site), which can occur up to 24 hours after drug administration.
- Most reactions were mild to moderate, and self-limited.
- Local reactions were the most common after the first rituximab/hyaluronidase injection. Incidence drops with subsequent injections.
Progressive multifocal Leukoencephalopathy: [US-Bound Warning]
- Patients receiving rituximab/hyaluronidase and rituximab-containing drugs may develop progressive multifocal leukoencephalopathy. This can include fatalities.
- Keep an eye out for neurological changes. Consider neurology consultation, brain MRI, and lumbar puncture if you suspect PML.
- Patients with PML should stop using it; you may want to reduce or discontinue concurrent chemotherapy and immunosuppressants.
Toxicity in the renal system:
- Can cause severe renal toxicities.
- Combination therapy with cisplatin/rituximab to treat NHL patients experienced renal toxicity during clinical trials. This combination is not approved.
- Tumor lysis syndrome can also cause renal toxicity.
- You should carefully assess your renal function and discontinue any rituximab products containing increased serum creatinine or oliguria.
Tumor lysis syndrome
- The rituximab product may cause tumor lysis syndrome within 12 to 24 hours.
- Hyperkalemia, hypocalcemia and hyperuricemia can all occur.
- Patients at high risk (high number of malignant cells >=25,000/mm3 and high tumor burden) should be given prophylaxis (antihyperuricemic treatment, hydration).
- If necessary, correct electrolyte imbalances; monitor renal function and hydration status and provide support if needed.
Rituximab and hyaluronidase (subcutaneous): Drug Interaction
Chloramphenicol (Ophthalmic) | May enhance the adverse/toxic effect of Myelosuppressive Agents. |
CloZAPine | Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. |
Coccidioides immitis Skin Test | Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. |
Denosumab | |
Local Anesthetics | Hyaluronidase may enhance the adverse/toxic effect of Local Anesthetics. Exceptions: Benzocaine; Benzydamine; Cocaine (Topical); Dibucaine; Dyclonine; Ethyl Chloride; Hexylresorcinol; Lidocaine (Ophthalmic); Lidocaine (Topical); Pramoxine; Proparacaine; Tetracaine (Ophthalmic); Tetracaine (Topical). |
Mesalamine | May enhance the myelosuppressive effect of Myelosuppressive Agents. |
Ocrelizumab | May enhance the immunosuppressive effect of Immunosuppressants. |
Pidotimod | Immunosuppressants may diminish the therapeutic effect of Pidotimod. |
Promazine | May enhance the myelosuppressive effect of Myelosuppressive Agents. |
Siponimod | Immunosuppressants may enhance the immunosuppressive effect of Siponimod. |
Tertomotide | Immunosuppressants may diminish the therapeutic effect of Tertomotide. |
Trastuzumab | May enhance the neutropenic effect of Immunosuppressants. |
Risk Factor D (Consider therapy modification) | |
Alpha-/Beta-Agonists | Hyaluronidase may enhance the vasoconstricting effect of Alpha-/BetaAgonists. Management: Avoid the use of hyaluronidase to enhance dispersion or absorption of alpha-/beta-agonists. Use of hyaluronidase for other purposes in patients receiving alpha-/betaagonists may be considered as clinically indicated. Exceptions: EPINEPHrine (Nasal); EPINEPHrine (Oral Inhalation); Isometheptene; Pseudoephedrine. |
Antihistamines | May diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving antihistamines (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. |
Corticosteroids | |
Deferiprone | Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. |
DOPamine | Hyaluronidase may enhance the adverse/toxic effect of DOPamine. Management: Avoid the use of hyaluronidase to enhance dispersion or absorption of dopamine. Use of hyaluronidase for other purposes in patients receiving dopamine may be considered as clinically indicated. |
Echinacea | May diminish the therapeutic effect of Immunosuppressants. |
Estrogen Derivatives | May diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving estrogens (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. |
Fingolimod | Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). |
Leflunomide | Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. |
Nivolumab | Immunosuppressants may diminish the therapeutic effect of Nivolumab. |
Roflumilast | May enhance the immunosuppressive effect of Immunosuppressants. |
Salicylates | May diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving salicylates (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. |
Sipuleucel-T | Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. |
Vaccines (Inactivated) | Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. |
Risk Factor X (Avoid combination) | |
BCG (Intravesical) | Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). |
BCG (Intravesical) | Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). |
Belimumab | May enhance the immunosuppressive effect of Biologic Disease-Modifying Antirheumatic Drugs (DMARDs). |
Biologic Disease-Modifying Antirheumatic Drugs (DMARDs) | May enhance the immunosuppressive effect of other Biologic Disease-Modifying Antirheumatic Drugs (DMARDs). |
Cladribine | May enhance the immunosuppressive effect of Immunosuppressants. |
Cladribine | May enhance the myelosuppressive effect of Myelosuppressive Agents. |
Dipyrone | May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased |
Natalizumab | Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. |
Phenylephrine (Systemic) | Hyaluronidase may enhance the vasoconstricting effect of Phenylephrine (Systemic). Management: Avoid the use of hyaluronidase to enhance dispersion or absorption of phenylephrine. Use of hyaluronidase for other purposes in patients receiving phenylephrine may be considered as clinically indicated. |
Pimecrolimus | May enhance the adverse/toxic effect of Immunosuppressants. |
Tacrolimus (Topical) | May enhance the adverse/toxic effect of Immunosuppressants. |
Vaccines (Live) | Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. |
Monitoring parameters:
- Patients at high risk of TLS may need electrolytes, CBC with differential, renal function (in patients who are at highest risk), fluid/hydration status balance, blood pressure, vital signs.
- Before starting therapy, screen all patients for HBV infection (eg, HBsAg or anti-HBc measures).
- Patients with evidence of hepatitis B infection, as well as carriers, should be closely monitored for signs and symptoms of HBV reactivation or infection. This monitoring can continue for up to two years after the end of therapy.
- Hepatitis B virus (HBV), screening recommendations (ASCO provisional Clinical Opinion Update):
- Before treatment initiation, screen for HBV infection using hepatitis B antigen (HBsAg), and hepatitis B antigen core antibody (antiHBc) tests. A total anti-HBc test (with both IgG/IgM) or anti HBc IgG test should also be performed to check for chronic or resolved HBV infections. Anti-HBc IgM may not confirm acute HBV infection.
- Patients with HBsAg and anti-HBc negative status should be tested for HBV reactivation by HBV DNA testing every three months.
- Monitor for hypersensitivity reactions for at least 15 minutes after administration
- Signs of active hepatitis B infection (during therapy and up to 12 months afterwards);
- Cardiac monitoring is performed during and after an infusion. This is for patients with pre-existing cardiac disease, or arrhythmias that develop during or following infusions.
- Monitor for intestinal obstruction/perforation (abdominal discomfort, vomiting);
- Multifocal leukoencephalopathy is a form of focal neurologic deficits. This can present as hemiparesis or visual field deficits. Cognitive impairments may also be present.
- TLS symptoms and/or mucocutaneous/cutaneous reactions are signs/symptoms.
How to administer Rituximab and Hyaluronidase (Rituxan Hycela)?
Only SubQ administration is possible.
- Avoid putting the cream on areas that are red, tender, hard or inflamed.
- If administration is interrupted, you can continue administration at the same site or at another location (restricted only to the abdomen).
- After administering rituximab/hyaluronidase, patients should be monitored for at least fifteen minutes.
- Avoid clogging the needle by attaching the injection needle immediately after administration.
- Rituximab/hyaluronidase works with both polypropylene, polycarbonate and stainless steel transfer needles and injection needles.
- It is best not to give it with any other subcutaneous medication.
Mechanism of action of Rituximab and Hyaluronidase (Rituxan Hycela):
Rituximab
- It is a monoclonal antibody which targets the CD20 antigen surfaced on pre-B and mature blood lymphocytes.
- CD20 antigens regulate cell cycle initiation and may function as calcium channels.
- Rituximab activates complement-dependent B cell cytotoxicity by binding to the antigen at the cell's surface. It also binds with the Fc receptors in humans, causing antibody-dependent cell toxicity.
Hyaluronidase
- It acts in a reversible manner at the site of administration, causing temporary depolymerization and increasing the permeability to the subcutaneous tissues.
- When administered in the recommended doses, it increases absorption of rituximab.
The beginning of action:
- CLL:
- After the first dose of rituximab patients' B-cells start to decline. 28% of them were depleted before the second cycle.
- Cycle 6: 96% of patients had B-cell depleted.
- FL
- After the first cycle, peripheral B-cell count drops to below normal. This is maintained throughout treatment with rituximab/hyaluronidase.
Duration of action:
- CLL:
- Patients remained B-cell depleted until month 9, where signs of repletion were seen.
- FL:
- After discontinuing rituximab/hyaluronidase, B-cell repletion begins after 6 months (may be longer in some patients)
Bioavailability of SubQ injection (compared to IV rituximab):
- CLL: 63.4%
- FL: 64.6%
Half-life elimination (terminal):
- CLL: 32 days
- FL: 34.1 days
International Brand Names of Rituximab and hyaluronidase:
- Rituxan Hycela
- Rituxan SC
- MabThera s.c.
- Mabthera SC
- Mabthera Solution for Subcutaneous Injection
Rituximab and hyaluronidase Brand Names in Pakistan:
No Brands Available in Pakistan.